Quick overview
Home insemination kits are sets intended for a single use at home: a syringe without a needle places the sample near the cervix. The approach is discreet and inexpensive, but only effective with good timing, clean technique and up‑to‑date testing. Neutral basics about the fertile window are provided by the NHS. For context on the chances and limits of home use see the HFEA.
Buying online – brief orientation
There are many ready-made home insemination kits online – from simple basic sets to comprehensive packages. Quality matters more than price: sterile single‑use parts, clear instructions, batch/expiry information and no cure claims. A complete kit is convenient if you want everything at once without researching. If you already have a syringe without a needle, a sterile cup, gloves and, if needed, sperm‑friendly gel organised cleanly, you don't need a kit – basic items suffice. Be cautious with “gimmicks” (activators, fragrances, reusable parts): no proven benefit and sometimes harmful.
What belongs in the kit?
- Sterile collection cup
- Syringe without needle (usually 5–10 ml), single‑use
- Disposable gloves
- Optional: pH‑neutral, sperm‑friendly lubricant
- Labels or bags for date, time, cycle day and notes

Kit types & components
| Component | Purpose | What to look for |
|---|---|---|
| Syringe without needle | Places the sample close to the cervix. | Single‑use, sterile, smooth plunger action; 5–10 ml is usually sufficient. |
| Soft applicator catheter | Sometimes included; facilitates gentle insertion. | Soft, flexible material; no sharp edges; single‑use. |
| Collection cup | Sterile collection of the sample. | Sterile packaging; do not rinse with disinfectants. |
| Sperm‑friendly lubricant | Can relieve dryness without greatly reducing motility. | Only products explicitly labelled as sperm‑friendly; use sparingly. |
| Ovulation test | Helps with timing of ovulation. | Clear instructions, check expiry date. |
| Checklists/labels | Better documentation per cycle. | Record date, time, cycle day and test results. |
Aggressive disinfectants, fragrances or reusable parts without sterilisation evidence are unnecessary.
Does it really work?
It can work, but outcomes vary widely. Key factors are age, precise timing, semen quality and care in technique. Clinics often achieve higher per‑cycle chances using prepared semen and tight timing compared with unprepared home use. For an impartial perspective see HFEA on insemination, Cochrane, and the NHS.
Purchase checklist & quality
- Sterile, individually packaged single‑use parts with clear batch and expiry information.
- Clear, factual instructions without cure claims.
- Information on hygiene, testing and disposal is included.
- Provider support contact is available.
- No dubious additives such as fragrances or “activators”.
Procedure in brief
- Plan timing around ovulation (ovulation tests/cycle tracking; see the NHS).
- Wash hands, put on gloves, prepare a clean surface; use only single‑use materials.
- Collect the sample sterilely and allow it to liquefy for 10–15 minutes.
- Slowly introduce the sample with the syringe close to the cervix; then rest quietly for 15–30 minutes.
- Document: date, time, cycle day and test results.
Quick overview – not personal medical advice.
Timing & practical tips
- Use the window around ovulation; plan several well‑organised cycles.
- Use lubricant only if necessary and then a designated sperm‑friendly product sparingly.
- Avoid extreme temperatures; use the sample promptly at room temperature.
- Lie back relaxed; avoid stress.
Safety & testing
- Prior testing for sexually transmitted infections for all involved (e.g. HIV, hepatitis, syphilis, chlamydia, gonorrhoea). Info: UKHSA and relevant clinical guidelines.
- Use only single‑use items; do not reuse anything.
- Do not allow disinfectant or soap residues to contact the sample.
- Seek medical advice for pain, bleeding or fever.
Where to get the sperm?
Sperm bank or clinic: Donor sperm is tested, documented and frozen. That increases safety and traceability. Further information: FPA.
Known donor: Possible, but without clinical standards there are more risks (infections, unclear responsibilities, missing documentation). Guidance on home use: HFEA.
If it doesn't work
First check the basics: ovulation was accurately targeted, technique was clean, the sample was fresh and not exposed to heat, and no ordinary lubricants were used. If pregnancy does not occur after several structured attempts, a medical assessment is worthwhile (cycle diagnostics, hormone status, ultrasound, semen analysis). Depending on findings, close cycle monitoring in a clinic or a clinic‑based insemination may be appropriate next steps. Neutral starting points: the NHS and the HFEA.
Gimmicks & myths
For home insemination kits, sterile single‑use parts and clean technique count – not accessories with big promises. A brief assessment of commonly mentioned “extras”:
- “Turkey baster”, pipettes, reusable parts: unsuitable and unhygienic. They lack sterility, fine control and documentation; they increase the risk of contamination.
- Menstrual/soft cups as a “reservoir”: sometimes discussed, but they show no reliable benefit over clean application with a syringe without a needle; handling and hygiene are more demanding.
- “Activators”, fragrances, oils, additives: no proven benefit and potentially harmful to sperm motility and survival.
- Heating devices/mats: too much heat damages sperm quickly; room temperature and prompt use are more important than gadgets.
- “Legs up/handstand”: popular but unsupported by evidence. Relaxed lying for 15–30 minutes is sufficient; comfort is preferable to acrobatics.
- Flushes or home remedies (e.g. bicarbonate, vinegar): do not use. They alter pH and can damage mucosa and sperm.
- Ordinary lubricants: can impede sperm. If needed, use only explicitly sperm‑friendly products very sparingly.
- Needle syringes or rigid catheters: do not use. If a catheter is included, it should be soft, flexible and single‑use.
Conclusion: a simple, clean set with a syringe without needle, sterile cup, gloves and clear instructions is superior to most “gimmicks”.
Home vs clinic
| Aspect | Home (kit) | Clinic (insemination) |
|---|---|---|
| Success per cycle | Wide range; depends on timing and baseline situation | Often higher with appropriate indication and prepared semen |
| Safety | Personal responsibility; risk of undetected infections | Standardised testing, documentation and traceability |
| Privacy/costs | Very private; low cost | Less private; higher cost, but structured care |
| Advice | Self‑research required | Medical advice and counselling included |
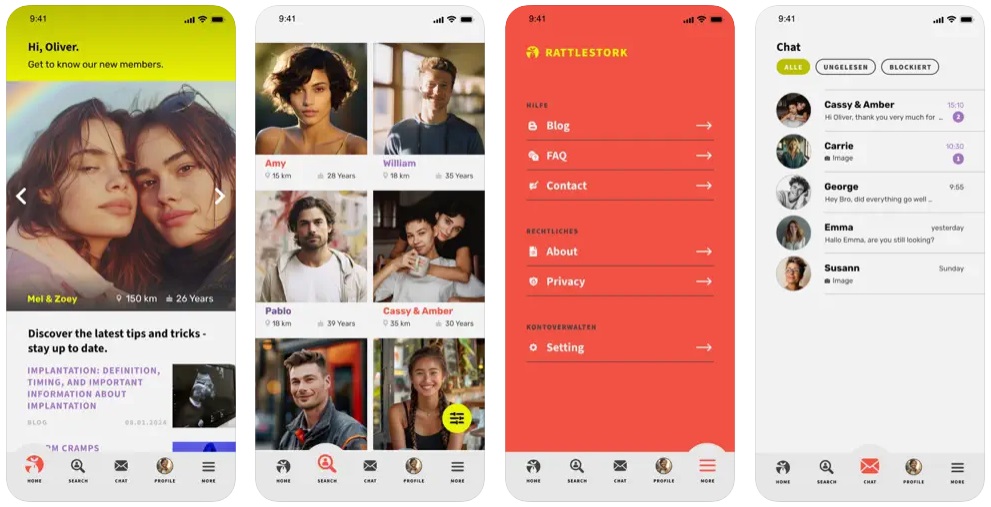
RattleStork – planning and coordination around sperm donation
RattleStork helps people plan family building responsibly. The platform offers verified profiles, secure communication and practical tools for organisation – appointment notes, cycle and timing entries and private checklists. RattleStork does not replace medical or legal advice but aggregates information and makes it easier to find suitable contacts.
Conclusion
Home insemination kits can help if timing, hygiene and testing are correct. Crucial are simple, sterile components and factual instructions – not the number of gimmicks. If several well‑planned cycles fail, seek medical assessment to determine sensible next steps. Helpful neutral starting points: the NHS, the HFEA, Cochrane, and UKHSA.

