Ovarian reserve (AMH & AFC) – your biological 'savings account'
The number of follicles is set at birth and declines throughout life. Two measures give a good overview of the remaining reserve:
- AMH (anti-Müllerian hormone): a blood marker that reflects the size of the active follicle pool. Low AMH suggests a smaller reserve, high AMH a larger one.
- AFC (antral follicle count): ultrasound count of small follicles at the start of the cycle; together with AMH it is informative for planning.
| Measure | What it shows | Typical use |
|---|---|---|
| AMH | Size of the follicle pool | Screening, monitoring, stimulation planning |
| AFC | Number of visible antral follicles | Ultrasound at cycle start, reserve estimation |
| FSH (day 2–5) | Pituitary regulation | Elevated = indicator of reduced reserve |
Interpretation should be carried out by experienced clinicians. NICE recommends structured investigations before treatment decisions are made.
Age & egg quality: what happens in the ovary
- Chromosome distribution: Aneuploidy increases with age, raising miscarriage risk and making implantation more difficult.
- Mitochondria & energy: Eggs from older people often have reduced 'energy reserves', which can affect early embryo stages.
- Hormonal dynamics: Cycle phases can shorten; the 'window' for implantation may become smaller.
- Overall effect: Lower reserve and lower egg quality explain why additional support is often useful from the mid-to-late 30s.
Numbers & success rates – realistic expectations
Natural chance per cycle: roughly 25–30% under 30, 10–15% at 35 and often <5% from 40. These ranges vary depending on cycle regularity, partner sperm quality and pre-existing conditions.
Miscarriage risk: increases with age (aneuploidy). Individual counselling is advisable, especially after recurrent miscarriages.
IVF/ICSI: Age-dependent success rates are reported in national registries; the CDC ART National Summary and the Success Estimator provide useful overviews.
Boosting egg quality – effective measures
- Not smoking: Tobacco accelerates ovarian ageing; quitting is beneficial immediately.
- Weight & metabolism: Aim for a stable BMI within the normal range and good insulin sensitivity.
- Alcohol & environment: Avoid heavy consumption; reduce exposure to endocrine disruptors (BPA/plasticisers).
- Sleep & shift work: Regular sleep patterns improve hormonal balance.
- Exercise & stress management: Moderate exercise, breathing and relaxation techniques.
- Partner check: A semen analysis clarifies whether male factors are involved.
Guidelines emphasise lifestyle interventions as a foundation — treatment options build on these (see NICE, NHS).
Testing fertility – AMH, AFC & cycle tracking
- AMH blood test: marker of reserve; sensible from the early 30s as a baseline, then repeat periodically.
- AFC ultrasound: count of antral follicles at cycle start; very helpful together with AMH.
- Cycle tracking: LH urine tests, basal body temperature, cervical mucus or wearables to pinpoint the fertile window.
- Additional diagnostics depending on findings: thyroid, prolactin, insulin resistance, vitamin D, coagulation; investigate for endometriosis if suspected.
Guidance: Under 35, seek medical advice after 12 months without pregnancy; from 35, after 6 months (recommendation e.g. NHS).
Social Freezing – procedure, chances & costs
Procedure
- 10–12 days of stimulation with daily injections
- Monitoring by ultrasound and hormone tests
- Egg retrieval under short anaesthesia (≈ 15 minutes)
- Vitrification at −196 °C
Success chances
The younger the eggs are at freezing, the higher the later chance per egg. Under 35, target ranges of about 12–20 eggs are often discussed; the success probability per egg decreases with age. Ethical and medical aspects: ESHRE guidance.
Costs
- Stimulation cycle: approx. €3,000–4,500
- Storage per year: approx. €200–300
- Reimbursement usually only for medical indications
For context on success rates, consult national registries, e.g. the CDC data.
Pre-existing conditions & risks – when to look more closely
Factors that may be relevant include: endometriosis (adhesions, pain), PCOS (ovulatory disorders, insulin resistance), thyroid dysfunction, hyperprolactinaemia, coagulation disorders (e.g. factor V Leiden). With cycle irregularities, severe pain, recurrent miscarriages or > 6–12 months of unsuccessful attempts to conceive, referral to a fertility clinic is advisable.
Your plan from today
- Baseline check: Have AMH & AFC measured in the coming weeks.
- Sharpen timing: Track 2–3 cycles with LH tests + basal temperature.
- Leverage lifestyle: Quit smoking, regular sleep, exercise, nutrition, reduce alcohol.
- Clarify options: Natural attempt vs IUI/IVF, possibly social freezing; arrange individual counselling.
- Check partner factor: Plan a semen analysis if appropriate.
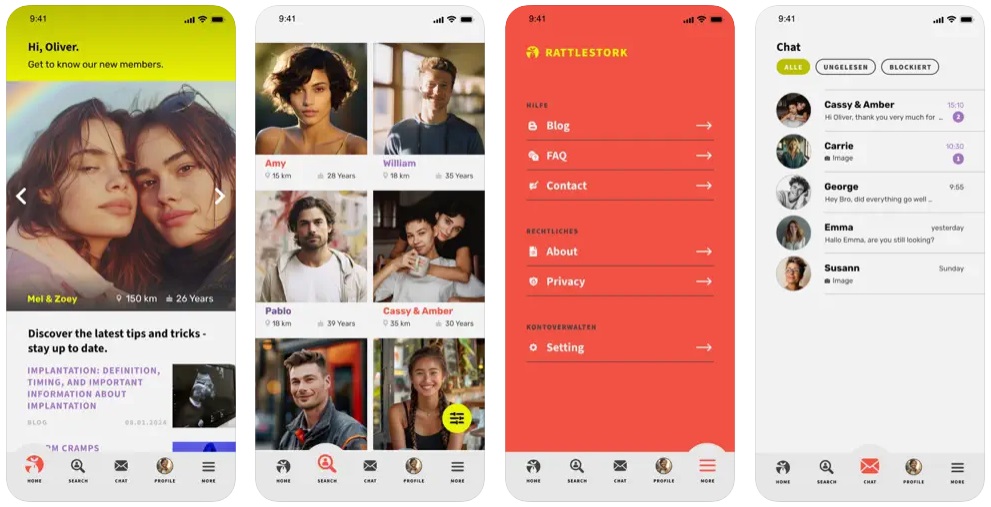
Sperm donation with RattleStork – option without a partner
If you lack a partner or male factors limit fertility, you can explore screened donor profiles, make contact and plan procedures via the RattleStork app — from anonymous donation to co-parenting or home insemination. This helps you make informed decisions suited to your situation.
Conclusion
You cannot stop time — but you can use it. Those who know their reserve and risks, optimise timing and evaluate options like social freezing or assisted reproduction calmly can measurably improve their chances. For orientation and planning see: WHO, NICE, NHS, CDC ART, ESHRE.

