Methods at a glance
- ICI / IVI – home insemination
Semen is placed with a syringe or cup near the cervix. Suits mild issues or donor sperm. Lowest cost, maximum privacy. - IUI – intrauterine insemination
Washed sperm is introduced via a thin catheter directly into the uterus. Useful for moderate male factor, cervical issues or unexplained infertility. - IVF – in vitro fertilisation
Multiple stimulated oocytes are combined with sperm in the lab. Standard for tubal factor or after unsuccessful IUI. - ICSI – sperm microinjection
A single sperm is injected into the oocyte. Preferred for severe male factor or TESE material.
In India, pricing varies widely between public institutes and private centres; medications and options (ICSI/PGT/cryostorage) are often billed separately.
Method cheat-sheets
| Method | Typical indication | Invasiveness | Cycle burden | Notables |
|---|---|---|---|---|
| ICI/IVI | Private donation, mild limitations | low | low | very private; timing is decisive |
| IUI | cervical factor, mild/moderate male factor, unexplained | low | low–medium | prepared sperm; day-care |
| IVF | tubal factor, endometriosis, after failed IUIs | medium | medium–high | lab fertilisation; single-embryo transfer preferred |
| ICSI | severe male factor, TESE | medium | medium–high | microinjection; higher lab component |
When each method makes sense
Choice depends on cause, age, ovarian reserve and history. Baseline work-up includes history, ultrasound, hormones and at least one semen analysis aligned with the WHO Semen Manual 2021.
- ICI/IVI: desired private donation, mild findings, strong preference for autonomy and privacy.
- IUI: thick cervical mucus, mildly/moderately altered semen parameters, unexplained infertility.
- IVF: blocked/absent tubes, significant endometriosis, IUI failures, combined factors.
- ICSI: markedly reduced sperm quality (OAT), azoospermia with TESE, failed fertilisation in IVF.
Setting success expectations
Outcomes hinge on age, diagnosis, gamete quality, embryo culture and transfer policy (single embryo). Patient-friendly explanations: NHS IVF page. For European best practice and safety standards see ESHRE.
How IUI, IVF & ICSI work
IUI in brief
Optional mild stimulation → semen preparation → thin catheter into the uterus around ovulation → possible luteal support.
IVF in brief
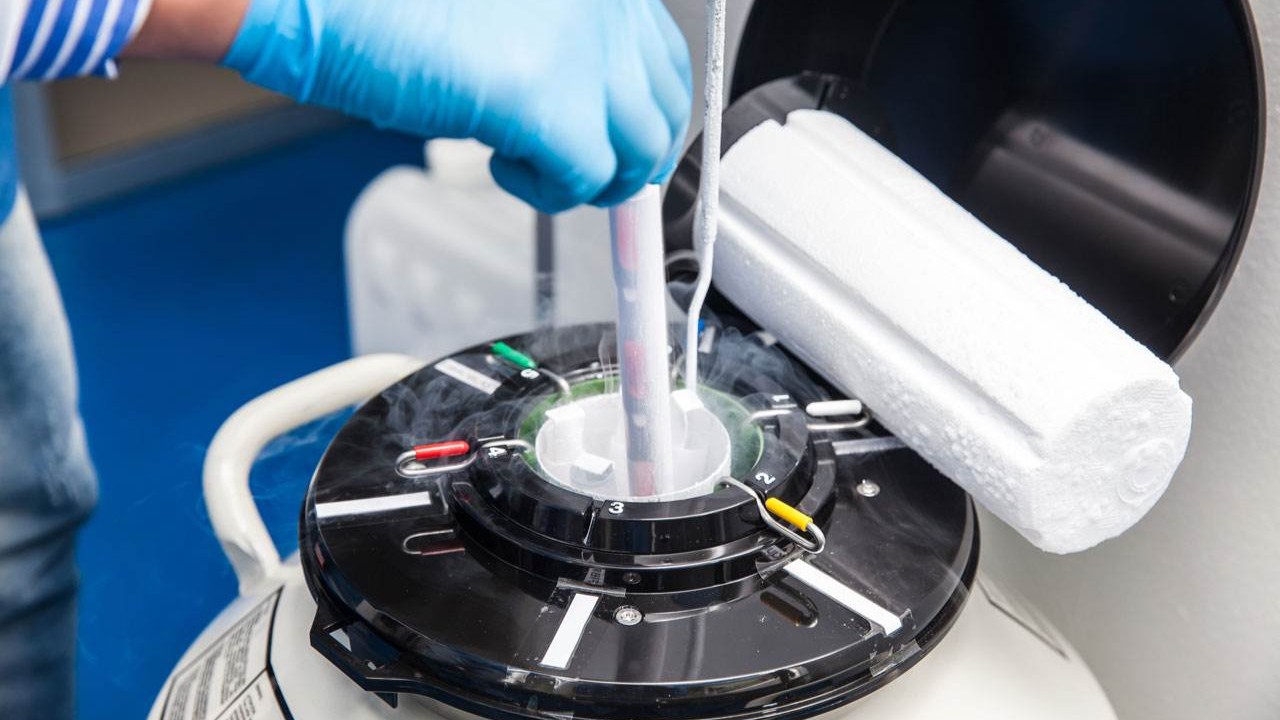
Stimulation with scan/blood monitoring → oocyte pickup → lab fertilisation → embryo culture → single-embryo transfer → cryo option for surplus.
ICSI in brief
As in IVF, but fertilisation via microinjection of a single sperm — especially for severe male factor.
Risks & safety
Usually mild, rarely severe: ovarian hyperstimulation syndrome (OHSS), bleeding/infection after pickup, multiple pregnancy risk with multiple-embryo transfer, psychological load. Individualised protocols and single-embryo transfer reduce risks markedly; see summaries and recommendations at ESHRE.
Costs & coverage (IN)
| Procedure | Typical components | Indicative range (₹) |
|---|---|---|
| IUI | mild stimulation (optional), prep, catheter, scans | ≈ ₹5,000–₹15,000 per cycle (private) |
| IVF | stimulation, pickup, fertilisation, culture, transfer | ≈ ₹1.2–₹2.5 lakh per cycle (+ medicines often ₹40,000–₹1.0 lakh) |
| ICSI | IVF + microinjection; higher lab share | add-on ≈ ₹30,000–₹80,000 |
| FET (frozen embryo transfer) | thawing, endometrium prep, transfer | ≈ ₹30,000–₹80,000; storage ≈ ₹5,000–₹20,000 per year |
Who pays? In the public sector, availability is limited to select institutes with eligibility criteria and waiting lists. In private care the patient typically pays out-of-pocket; some insurers offer partial benefits for specific steps per policy terms, but many plans exclude infertility treatment. Always request a written, itemised quote with inclusions/exclusions (procedures, drugs, cryo/storage, options) and price validity.
Legal framework (IN)
ART is provided in registered clinics under Indian law and professional standards. The Assisted Reproductive Technology (Regulation) Act, 2021 governs clinic/Bank registration, consents, screening, records and oversight. Gamete donation is permitted under regulated conditions with mandatory testing and documentation. Surrogacy is allowed only on an altruistic basis under the Surrogacy (Regulation) Act, 2021 with strict eligibility and approvals. Always confirm current requirements with your centre.
Checklist before you start
- Complete baseline work-up (hormones, ultrasound, semen per WHO 2021).
- Agree the indication and goal (e.g., single-embryo transfer as default; cryo strategy).
- Understand medication & monitoring; note emergency contacts.
- Validate costs, any insurance/government support, recurring fees (storage, options).
- Plan psychological support and pauses between cycles if needed.
Alternatives & add-ons
Depending on your baseline, cycle tracking, precise timing and lifestyle measures can help. If donor sperm is preferred or an ICI/IVI path fits you better, explore our tools and guides.
- ICI / IVI – home insemination: plan autonomously and discreetly.
- IUI: day-care option with prepared sperm.
- IVF: lab fertilisation for tubal factor or after IUI.
- ICSI: key for severe male factor.
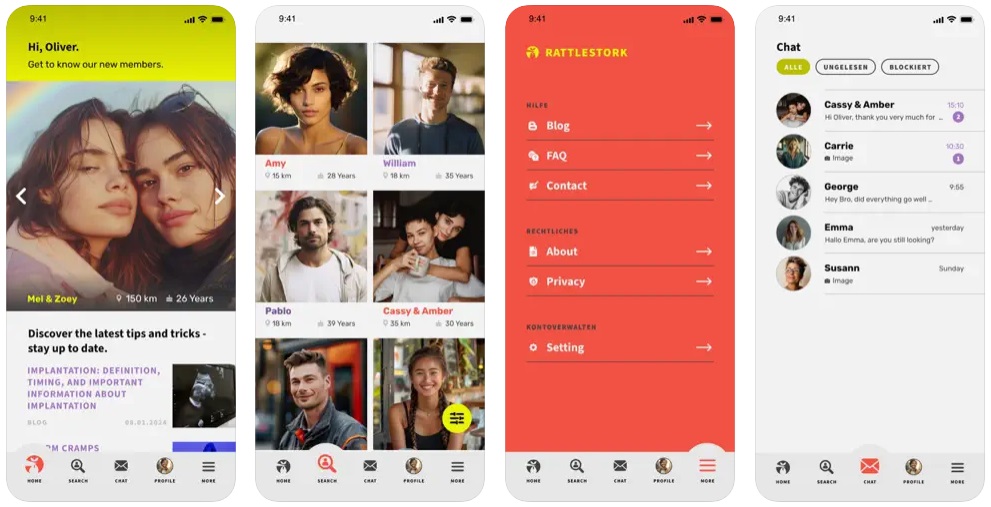
RattleStork — plan safely, document clearly
RattleStork supports you with verified profiles, secure chat, and tools for appointments, cycle/timing notes and private checklists — helpful for private sperm donation (ICI/IVI) and structured decision-making. RattleStork does not replace medical advice.
Takeaway
ART offers multiple paths — what matters is sound diagnosis, a realistic plan and clear information. See our pages on ICI/IVI, IUI, IVF and ICSI to prepare your next step confidently.