Methods at a glance
- ICI / IVI — at-home insemination
Semen placed with syringe or cup near the cervix. Good for mild factors or donor sperm. Lowest cost, highest privacy. - IUI — intrauterine insemination
Washed sperm guided by catheter into the uterus. Used for moderate male factors, cervical issues or unexplained infertility. - IVF — in vitro fertilization
Multiple stimulated oocytes fertilized in the lab. Standard for tubal factor or after unsuccessful IUI. - ICSI — sperm micro-injection
A single sperm is injected into the oocyte. Best for severe male factor or TESE material.
In Canadian private clinics, a non-funded IVF cycle commonly totals ~$10,000–$15,000 CAD for the procedure, with +$3,000–$7,000 CAD for medications; add-ons (ICSI/PGT/freezing) are extra.
Method quick profiles
| Method | Typical indication | Invasiveness | Cycle burden | Notes |
|---|---|---|---|---|
| ICI/IVI | Private donation, mild limitations | low | low | very private; timing critical |
| IUI | cervical factor, mild/moderate male factor, unexplained | low | low–medium | washed sperm; outpatient |
| IVF | tubal factor, endometriosis, after IUI failures | medium | medium–high | lab fertilization; single-embryo transfer preferred |
| ICSI | severe male factor, TESE | medium | medium–high | micro-injection; higher lab share |
When each method makes sense
Choice depends on cause, age, ovarian reserve and history. Baseline work-up includes history, ultrasound, hormones and at least one quality-assured semen analysis per the WHO Semen Manual 2021.
- ICI/IVI: desired private donation, mild deviations, high autonomy/privacy.
- IUI: thick cervical mucus, mild/moderate semen deviations, unexplained infertility.
- IVF: blocked/absent tubes, significant endometriosis, after IUI, combined factors.
- ICSI: markedly reduced sperm quality (OAT), azoospermia with TESE, failed fertilization in IVF.
Understanding success realistically
Outcomes depend on age, diagnosis, gamete quality, embryo culture and transfer policy (single-embryo). Patient-friendly explanations: NHS; European best-practice via ESHRE.
How IUI, IVF & ICSI work
IUI in brief
Optional mild stimulation → sperm prep → thin catheter into the uterus near ovulation → possible luteal support.
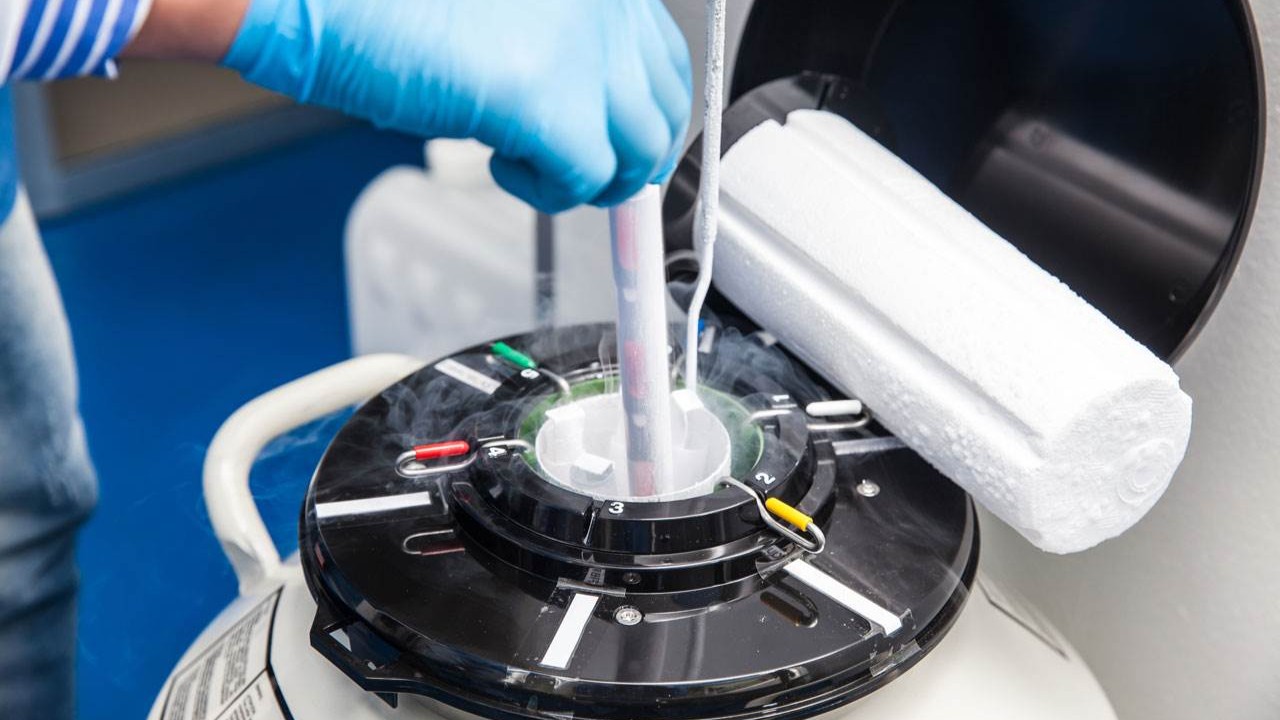
IVF in brief
Stimulation with US/blood monitoring → egg retrieval → lab fertilization → embryo culture → single-embryo transfer → cryo options for remaining embryos.
ICSI in brief
As IVF, but fertilization via micro-injection of one sperm into the oocyte — especially for severe male factor.
Risks & safety
Mostly mild, rarely severe: ovarian hyperstimulation syndrome (OHSS), bleeding/infection after retrieval, multiples risk with multi-embryo transfer, psychological strain. Individualized protocols and single-embryo transfer reduce risks; see ESHRE for summaries.
Costs & coverage (Canada)
| Procedure | Typical items | Approx (CAD) |
|---|---|---|
| IUI | optional stimulation, sperm prep, catheter, monitoring | ~$500–$1,500 per cycle (private); meds extra |
| IVF | stimulation, retrieval, fertilization, culture, transfer | ~$10,000–$15,000 per cycle (procedure only) |
| ICSI | IVF plus micro-injection; higher lab share | +~$1,500–$3,000 add-on |
| Cryo transfer | thaw, endometrium prep, transfer | ~$2,500–$4,000; storage often $500–$1,500/yr |
Public funding/tax credits (snapshot, verify locally):
- Ontario (OFP): 1 publicly funded IVF cycle per eligible patient lifetime (under 43; OHIP; participating clinics). IUI procedures are funded; meds/ancillaries often not. Details vary by clinic.
- Québec (RAMQ): 1 covered IVF cycle for eligible patients (female <41 at retrieval); transfers from that cycle covered up to 42 years minus 1 day; up to 6 IUIs for ages 18–40.
- New Brunswick (FTRP): reimbursement program — up to ~$10,000 for IUI and ~$20,000 for one IVF cycle per household.
- Manitoba (FTTC): refundable tax credit equal to 40% of eligible fertility expenses; annual claimable eligible costs increased to $40,000 (max credit $16,000 for 2024 tax year onward).
- Nova Scotia: Fertility & Surrogacy refundable tax credit at 40% of eligible costs (annual caps apply).
- Federal supports: Medical Expense Tax Credit (METC) and NIHB (case-by-case medication coverage for eligible First Nations and Inuit).
Always request written price plans and funding eligibility from your clinic and your province/territory, including what’s excluded (medications, diagnostics, storage, add-ons).
Legal framework (Canada)
Assisted reproduction is governed federally by the Assisted Human Reproduction Act (altruistic surrogacy only; strict rules on gamete/embryo handling and compensation limits). Delivery of care, age limits and public funding are set provincially/territorially. Clinics follow national standards and report to provincial bodies; parentage rules vary by province/territory (seek local legal advice where needed).
Pre-treatment checklist
- Complete baseline work-up (hormones, ultrasound, semen per WHO manual).
- Define indication & goal (e.g., single-embryo transfer by default; cryo strategy).
- Understand meds and monitoring; record urgent contacts.
- Get written cost plan; confirm provincial funding/tax credits and any payment plans.
- Line up mental health support; schedule intentional breaks.
Alternatives & complements
Depending on your profile, cycle tracking, precise timing and lifestyle changes can help. If donor sperm is desired or an ICI/IVI path fits you, you’ll find deeper info and tools here.
- ICI / IVI — at-home insemination: plan autonomously and privately.
- IUI: outpatient option with washed sperm.
- IVF: lab fertilization for tubal factor or after IUIs.
- ICSI: for markedly reduced sperm quality.
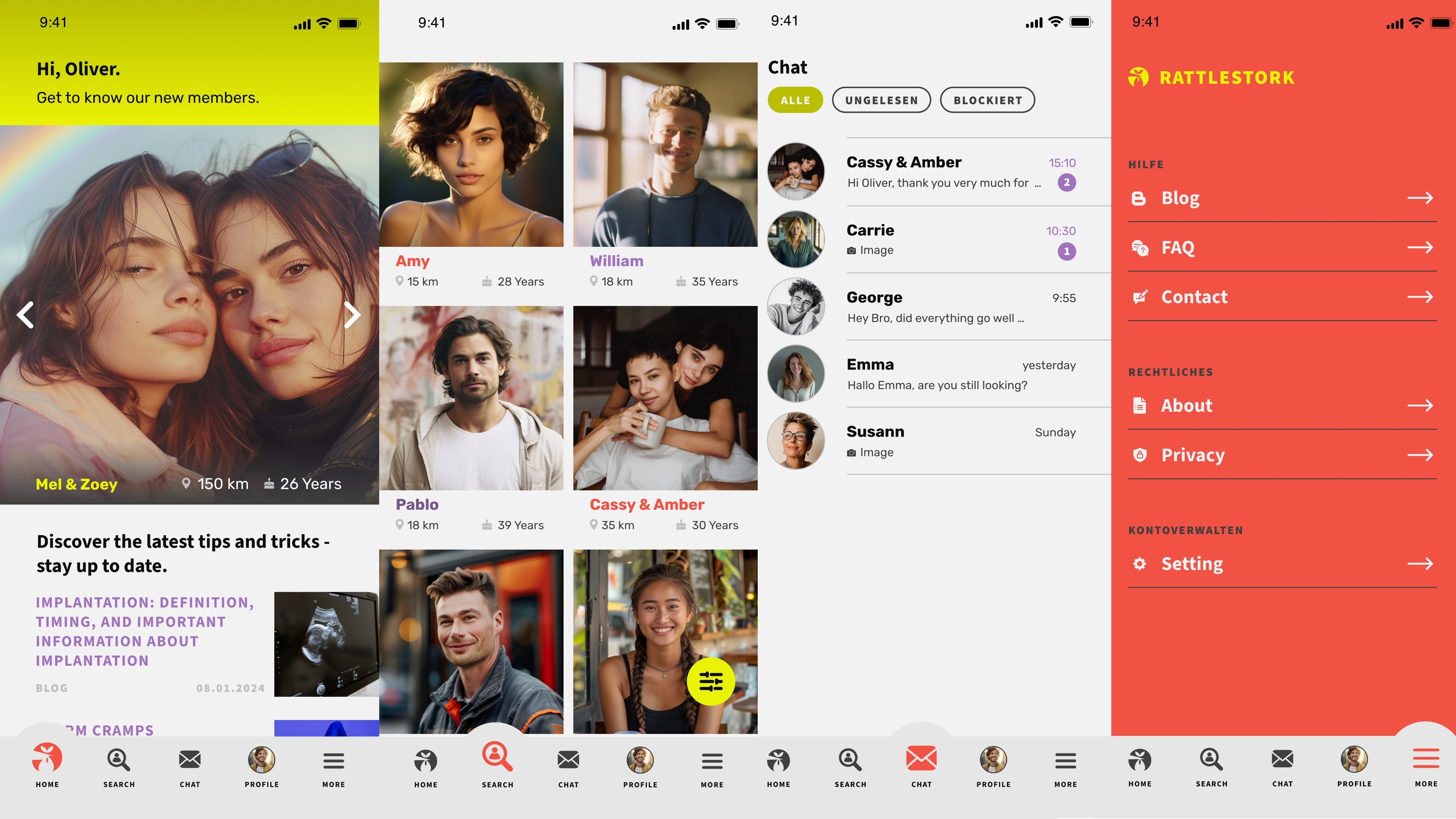
RattleStork — plan safely, document well
RattleStork supports you with verified profiles, secure messaging and tools for appointments, cycle & timing notes, and private checklists — helpful for private donation (ICI/IVI) and structured decision-making. RattleStork does not replace medical advice.
Conclusion
Assisted reproduction offers many paths. The key is a sound diagnosis, a realistic plan and clear information. Use our sections on ICI/IVI, IUI, IVF and ICSI to take the next step with confidence.