Context
RattleStork facilitates contacts and knowledge. We do not ship samples and we do not carry out transports. This article explains how to move fresh ejaculate safely and practically from A to B, which packaging and carrying method make sense, and where the limits are.
Transport basics
The goal during transport is consistency: short routes, body-near temperature, calm positioning. Sperm are sensitive to heat, cold, and long waits. The WHO laboratory manual recommends short intervals between collection and processing and protection from temperature spikes. WHO Laboratory Manual 2021.
- Temperature: aim for roughly 68–98.6 °F; avoid hot or cold sources.
- Position: carry the cup upright and tightly closed.
- Stability: avoid shaking; normal walking is fine, vigorous shaking is not.
- Privacy & discretion: place the cup in a small bag, then carry it close to the body (inside pocket).
Short-distance transport: step by step
- Use a sterile specimen cup with a wide opening and a tight lid (ideally provided by the clinic). Collect the full ejaculate and note the time. Guidance on cup selection can be found in ESHRE lab standards. ESHRE IVF-Lab Guideline
- Secondary packaging: place the cup into a clean, tightly sealing bag (leak protection), then carry in an inside pocket or firmly against the body.
- Carrying: upright, close to the body, away from sun, warm heater air, and drafts. Do not use a heating pad, cold packs, or a microwave.
- Route & transport: on foot or by car without heated seats; bicycle only with care. Choose a direct route and avoid stops.
- Hand-over: confirm opening hours and the acceptance process in advance; tell the lab the collection time. Many centers issue clear transport notes (keep warm, drop off promptly). Examples: NHS leaflet, UCLH guidance
Tip: take a spare bag. If the lid gets wet on the outside, wipe it—do not heat it.
Avoiding temperature traps
- Cold: winter air, cool packs, or a refrigerator reduce motility. Solution: carry close to the body. UCLH
- Heat: heating pads, heated seats, direct sun, and heater vents are harmful. NHS leaflet
- Wrong containers: condoms and many lubricants are spermicidal; use only sterile, suitable specimen cups. ESHRE
What is not recommended
- Leaving the cup to “temper.” Passive storage often leads to cooling down or overheating.
- Fridge, freezer, ice, or hot water.
- Non-sterile containers or containers with additives. Always use sterile specimen cups. ESHRE
Typical myths & clarifications
- Electric blanket helps: too hot locally. Carrying close to the body is sufficient.
- Cool pack keeps it “fresh”: cold slows movement.
- “Warm up” under tap water: moisture and thermal shock are risky.
Cryo shipping & professional couriers
For long distances or longer timeframes, cryopreservation in nitrogen vapor (dry shipper, around −238 to −320 °F) is the standard. Clinic-to-clinic transfers and international movements are regulated; approved facilities and processes are required. HFEA explains permissions and procedures. HFEA Import/Export. For storage practice: UCLH sperm storage.
Comparison: human medicine vs. animal breeding
In cattle breeding, pre-frozen straws are stored in liquid nitrogen (−320 °F) and transported in the field with dry shippers; before insemination they are briefly thawed in water at about 95–102 °F. This setup requires protective measures and trained staff. FAO: Cryoconservation.

These protocols cannot be transferred to private human applications. Human centers work with identity checks, infection screening, and clear legal requirements; private shipping without approval is risky.
Time windows
The following ranges are typical practice values; your center’s specific instructions are decisive.
| Situation | Time window | Target temperature | Notes |
|---|---|---|---|
| Semen analysis/diagnostics (drop-off at laboratory) | 30–60 min, sometimes up to 2 h | close to body, approx. 68–98.6 °F | Carry upright, avoid extremes. UCLH |
| Post-vasectomy check | often ≤ 1 h, locally up to 2–4 h | close to body | The quicker, the more reliable the motility assessment. NHS Andrology |
| Home insemination (ICI) | as fresh as possible, ideally under 60 min | close to body | Single-use materials, hygiene, up-to-date STI status. WHO 2021 |
Many clinics state clearly: keep warm, drop off promptly, avoid extreme temperatures. Examples: NHS Wrightington, Gloucestershire Hospitals.
Legal & clinic practice
Clinics define acceptance windows, suitable containers, and identity checks. For cross-border movements, authorities such as the HFEA refer to licensed clinics and specialist couriers. HFEA – using donated gametes.
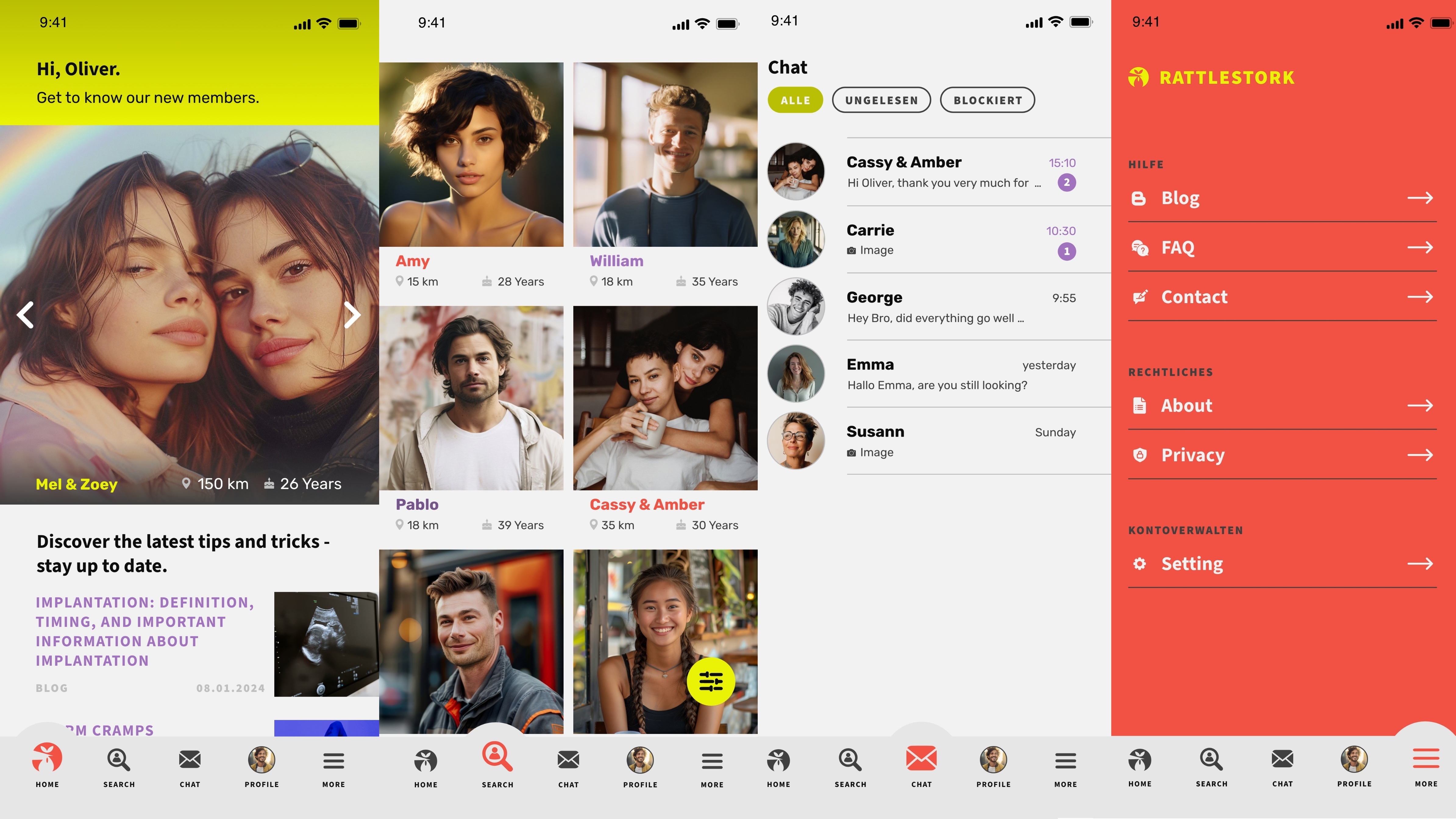
RattleStork – plan transparently
RattleStork helps you structure planning steps clearly: verified profiles, secure exchange, notes for appointments, cycle and timing, plus private checklists. We are not a delivery service and do not provide medical services, but we help you understand the process and make informed decisions.
Conclusion
Safe transport starts with a sterile specimen cup, secondary packaging, and carrying close to the body. Keep it calm, upright, and away from heat or cold spikes—then drop off promptly. For longer distances, cryopreservation and professional couriers are the standard. RattleStork does not deliver, but provides tools and knowledge to plan the process properly.

