Decision first
Before appointments and medicines, decide roles: who donates, who carries—and why. Key inputs are egg age and findings, day-to-day practicality, and your shared preference. A simple decision matrix helps:
| Criterion | Questions to assess | Practical tip |
|---|---|---|
| Egg factors | Age, AMH/AFC, endometriosis, previous surgery | Align roles with egg age |
| Uterine factors | Lining, fibroids/polyps, inflammation | Address issues before starting |
| Work & life | Work hours, shifts, care support | Share calendars and plan cover |
| Preference & roles | Who prefers to donate, who to carry—now & later? | Discuss expectations openly |
How reciprocal IVF works
Partner A’s eggs are stimulated and collected, fertilized in the lab with donor sperm, and the embryo is transferred to Partner B’s uterus. A contributes the genetics, B the pregnancy. For a future sibling, you can intentionally swap roles. The clinical pathway mirrors IVF; the main differences are role allocation, documentation and legal steps.

Success rates and factors
The strongest lever is the egg age of the donating partner. Other drivers include lab quality, embryo development, endometrial preparation, transfer timing, a single-embryo strategy, and co-existing conditions. ASRM guidance emphasizes single-embryo transfer for many patients to reduce multiple pregnancy risks; check your clinic’s SART/CDC data and protocols (ASRM; CDC ART).
| Factor | Impact | What to do |
|---|---|---|
| Egg age | high | Use age & AMH/AFC to inform role choice |
| Embryo quality | moderate–high | Choose an experienced SART-member clinic; avoid unproven add-ons |
| Endometrium | moderate | Treat inflammation/fibroids; hit the transfer window |
| Transfer strategy | moderate | Default to single-embryo transfer where appropriate |
| Lifestyle | moderate | Don’t smoke; prioritize sleep, nutrition and stress care |
Donor screening and tissue establishment standards are set by the FDA (21 CFR Part 1271); reputable banks and clinics follow these rules (21 CFR 1271; FDA donor eligibility guidance).
Step-by-step
Pre-assessment for both: Medical history, ultrasound, hormones, ovarian reserve (AMH/AFC), infection screening, vaccination review; genetic counselling if needed. Set roles, timeline and budget; select a SART-member clinic.
Ovarian stimulation and egg collection (Partner A): Stimulation with monitoring, trigger, transvaginal collection. Aim: good yield with a low OHSS risk.
Fertilization and embryo culture: IVF/ICSI depending on findings, culture over several days, quality grading. Use add-ons only where benefit is evidenced.
Preparing for transfer (Partner B): Lining preparation in a natural or substituted cycle; define the transfer window; usually single-embryo transfer.
Transfer and follow-up: Embryo transfer, luteal support, pregnancy test, early scan; adjust medicines where needed.
Safety, tests and medicines
Standard care includes up-to-date infection screening, vaccination status (e.g., rubella), medicine and thyroid checks, and folic acid pre-conception. Modern protocols reduce OHSS risk; single-embryo strategies cut multiple pregnancy risk. See ASRM’s clinical guidance for embryo transfer techniques and patient selection (ASRM embryo transfer guideline).
Time, costs and organisation
Expect a wait for the first appointment and diagnostics. The active phase typically spans two to six weeks—from stimulation through collection and culture to transfer. Costs vary by state, clinic and protocol; plan headroom for medicines, possible frozen transfers and storage. Insurance coverage depends on your state’s mandate and your plan—start with RESOLVE’s state coverage overview and your HR benefits portal (RESOLVE: coverage by state).
| Building block | What to consider | Practical tip |
|---|---|---|
| Appointments | Monitoring, procedure day, transfer window, time off work | Shared calendar; arrange cover early |
| Budget | Stimulation, collection, lab, transfer, medicines; possible freezing & storage | Request itemized quotes; add contingency |
| Documents | Consents, donor papers, invoices, protocols | Scan and store centrally for the long term |
| Logistics | Travel, childcare, day-to-day support | Use checklists; define responsibilities |
Choosing a donor
You may use a clinic/sperm-bank donor or a known donor. Prioritize current testing, transparent profiles, clarity on future contact, and robust documentation. If you plan siblings, discuss same-donor availability and family limits early. In the U.S., donor screening and tissue establishments are regulated by the FDA (21 CFR Part 1271). Choose banks and clinics that follow these rules and publish clear policies on identity-release options (FDA guidance).
Legal basics (USA)
Parentage & recognition: U.S. parentage law is state-based. In many states, a married non-gestational parent in a same-sex marriage is recognized at birth; however, confirm with your attorney and consider a confirmatory adoption or parentage judgment for cross-state security. Sperm donors used via licensed clinics are typically not legal parents, but details vary by state statute and case law.
Clinic & donor regulation: Clinics report to CDC/SART; donors and tissue establishments follow FDA HCT/P rules (21 CFR Part 1271) on screening, testing and records (CDC ART rates; SART; 21 CFR 1271).
Insurance & benefits: Coverage depends on state mandates and your plan type (ERISA-self-insured plans are often exempt). Start with RESOLVE’s state tracker and your HR plan documents (RESOLVE state coverage).
Practical note for reciprocal IVF: IVF with donor sperm is medically feasible; ensure your consent forms reflect roles (genetic vs. gestational parent) and keep copies of all records. Because rules differ by state, get tailored legal advice before starting.
Myths and facts
- More embryos mean higher chances? Single-embryo transfer reduces risk and is often the safer strategy.
- The fitter partner should carry? Egg age, medical history, daily life and preference matter more.
- Add-ons always help? Only use those with proven benefit.
- Law is the same everywhere? U.S. laws vary by state; check your jurisdiction.
- Fresh beats frozen? Frozen transfers can perform just as well.
- Lifestyle cancels out age? Healthy habits help but don’t replace biology.
- A known donor makes everything simpler? Testing, documentation and clear agreements remain essential.
- One negative transfer means the plan was wrong? Several attempts are common; protocols can be adjusted.
When to see a doctor
- Before starting: baseline assessments plus role and timeline planning.
- If you have existing conditions, take regular medicines or have cycle irregularities.
- If pregnancy doesn’t occur after transfers or protocols need changing.
U.S. context: review your clinic’s CDC/SART data, confirm FDA-compliant donor sourcing, and align with ASRM guidance on embryo transfer (CDC ART; ASRM).
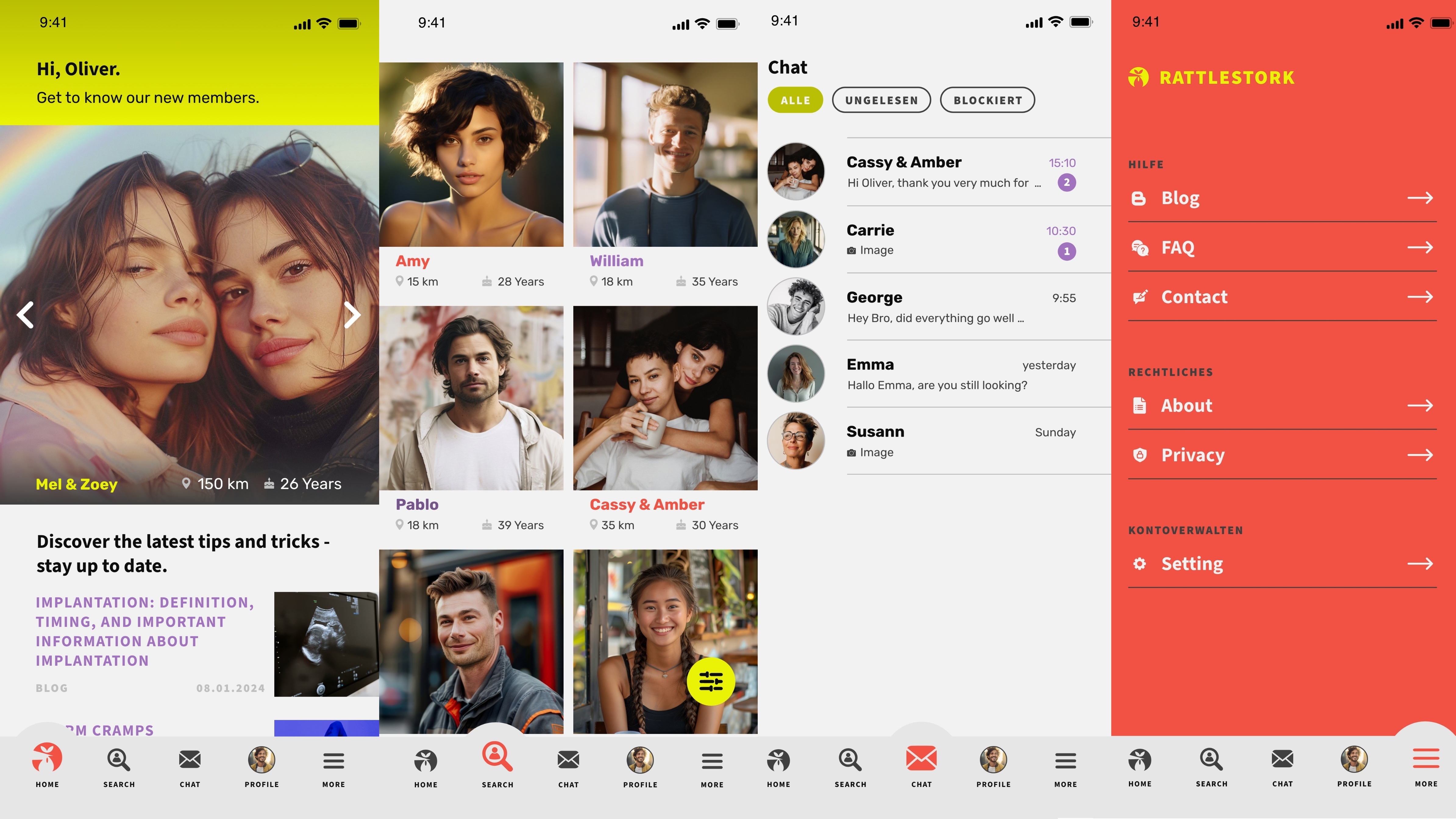
Find donors with RattleStork
RattleStork helps you search for donors with verified profiles, secure messaging and tools for scheduling, notes, cycle and timing planning, plus private checklists. Focus: transparency, safety and sound documentation. RattleStork is not a substitute for medical advice.
Conclusion
Reciprocal IVF combines shared involvement with the structure of clinical care. What matters most: egg age, a well-prepared endometrium, realistic time and budget plans, evidence-based choices and the right paperwork. In the U.S., check state-specific laws and insurance rules early, verify clinic quality via CDC/SART, and keep thorough documentation from the start.

