What is an ectopic pregnancy
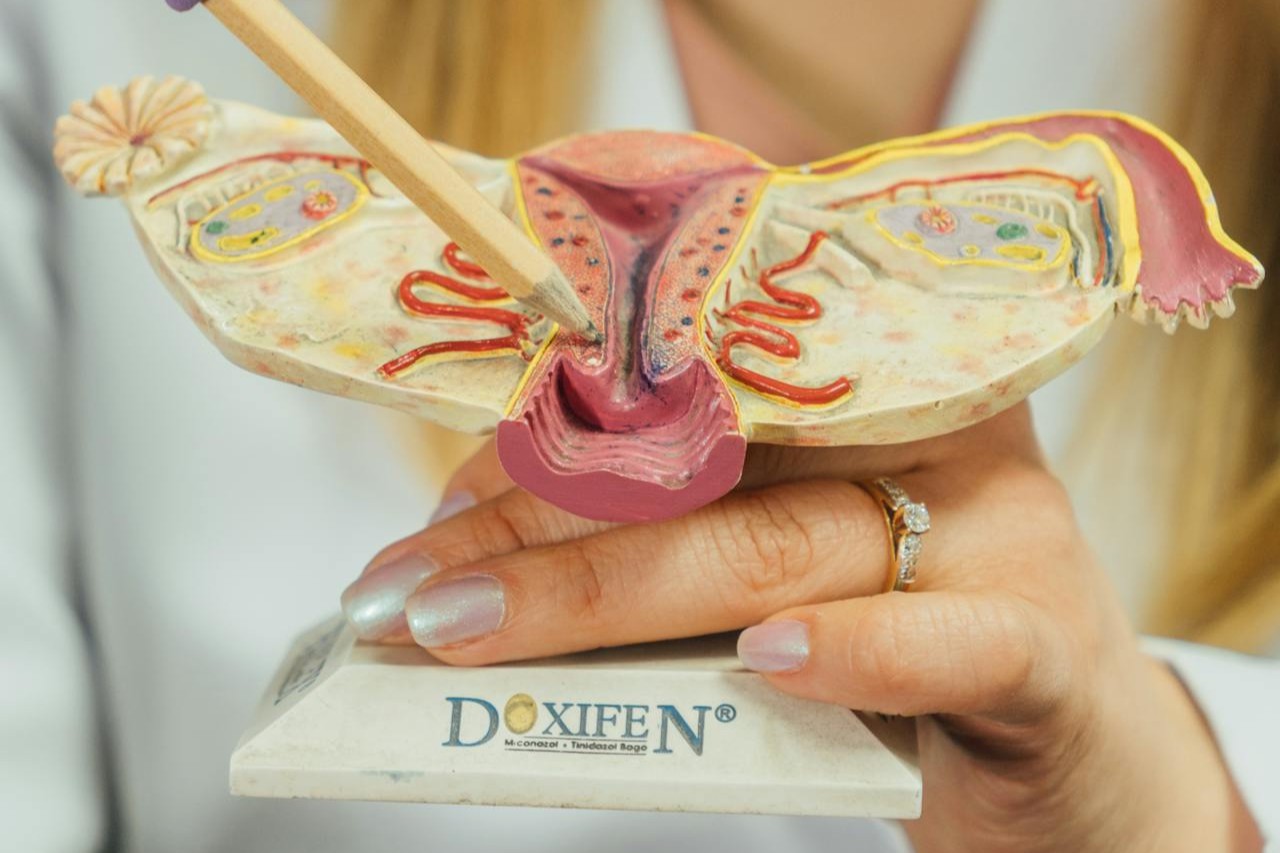
In an ectopic pregnancy, the fertilized egg implants outside the uterus, most commonly in the fallopian tube. Medically, it is classified as an extrauterine pregnancy, meaning a pregnancy located outside the uterine cavity.
The most frequent location is the fallopian tube. Less commonly, implantation can occur in the ovary, the cervix, a cesarean scar, or the abdominal cavity. Patient information resources summarize these forms in an accessible way. RCOG: Ectopic pregnancy.
Why it happens
After fertilization, the egg must be transported through the fallopian tube to the uterus. If this transport is disturbed, implantation in the fallopian tube can occur. It is rarely a single cause and is often a combination of anatomical and functional factors.
Common factors that increase the risk include:
- previous ectopic pregnancy
- pelvic inflammation or prior infections, especially if the fallopian tubes were affected
- surgeries on the fallopian tubes or abdomen that caused adhesions
- endometriosis
- smoking
- pregnancy while using an intrauterine device or after sterilization—rare but with a higher proportion of extrauterine cases
- assisted reproduction, often due to underlying factors and closer diagnostic surveillance
Important: An ectopic pregnancy can occur even without identifiable risk factors. This is not unusual and is not a sign of personal fault.
How common it is
Depending on the country and data source, ectopic pregnancies account for roughly one to two percent of all pregnancies. The clinical significance is high because untreated cases can lead to internal bleeding.
Symptoms: what is typical and what can be an emergency
An ectopic pregnancy may cause few or no symptoms at first. When symptoms occur, they are often nonspecific. That is why the combination of pregnancy test, clinical course, and ultrasound is so important.
Common warning signs include:
- lower abdominal pain, often one-sided, sometimes increasing
- spotting or bleeding outside a normal period
- shoulder-tip pain, especially when accompanied by nausea or lightheadedness
- dizziness, weakness, fainting, or circulatory problems
Severe pain, increasing bleeding, or circulatory symptoms always warrant immediate medical evaluation. A clear description of typical symptoms and emergency signs is available from the NHS. NHS: Symptoms of ectopic pregnancy.
Why it is not viable
The fallopian tube is not designed to carry a pregnancy. It cannot expand like the uterus and does not provide the appropriate structure for a stable placental blood supply. Therefore, an ectopic pregnancy cannot continue to term.
If left untreated, the fallopian tube can rupture. This is a medical emergency with a risk of internal bleeding.
Diagnosis: how clinicians logically assess it
The diagnosis rarely rests on a single finding. The key is the combination of symptoms, serial hCG measurements, and transvaginal ultrasound. In very early weeks, the ultrasound may not yet show definitive findings. In those cases, the pregnancy may be labeled as a pregnancy of unknown location until the course becomes clear.
Typical elements of evaluation include:
- serial quantitative hCG measurements rather than a single value
- transvaginal ultrasound to examine the uterus and adnexa
- clinical assessment of pain, bleeding, and circulatory status
The practical point is simple: a positive pregnancy test alone does not tell you where the pregnancy is located. If the hCG trend and ultrasound do not match, close follow-up is required. A practical clinical overview of diagnosis and management is provided by the AAFP. AAFP: Ectopic pregnancy diagnosis and management.
Treatment: what may be appropriate in different situations
Treatment depends on stability, findings, hCG level, ultrasound signs, and your individual situation. The goal is always safety—preventing complications—while treating as conservatively as possible.
Expectant management
If you are stable, symptoms are mild, and hCG is falling on its own, expectant management may be an option. That does not mean doing nothing, but rather scheduled follow-up until the trend is clearly resolving.
Medical treatment with methotrexate
When criteria are met, methotrexate can be used to stop the pregnancy tissue without surgery. Reliable follow-up is essential because hCG must be monitored over time and any new pain must be reassessed.
In practice, methotrexate is mainly appropriate when the clinical course is stable and there are no signs of an acute emergency. ACOG explains the approach and basic principles in patient-oriented guidance. ACOG: Ectopic pregnancy.
Surgical treatment
Surgery is required if you are unstable, if a rupture is suspected, or if the findings make a medical approach unlikely to succeed. Surgery is often performed minimally invasively. Depending on the situation, the surgeon may remove the pregnancy tissue and either conserve part of the tube or remove the tube entirely.
The choice depends on the findings, bleeding, condition of the tube, and your fertility desires. There is rarely a perfect solution—usually a balance of risks.
After treatment: hCG, the body, and recovery
Recovery after an ectopic pregnancy often has two aspects. The body needs time to heal and for hCG levels to normalize. At the same time, the experience can be emotionally challenging even when the medical outcome is good.
Common practical considerations include:
- follow-up until hCG is negative again, depending on the approach
- a plan for when pain is expected to be normal and when it requires reassessment
- with methotrexate, clear guidance on timing before the next pregnancy, often including folate management
- after surgery, wound healing, graduated return to activity, and postoperative care
If you feel persistently low, anxious, or overwhelmed for weeks afterward, that is not a sign of weakness. It is a valid reason to seek support.
How it may affect future fertility
An ectopic pregnancy does not automatically mean future pregnancy is impossible. Many people conceive normally afterward. How soon it is reasonable to try again depends on the treatment and your individual situation.
A practical plan often helps: first confirm hCG is clearly negative, then allow physical recovery, and in a new pregnancy check early by ultrasound to confirm the location in the uterus.
Risk of a repeat ectopic pregnancy
The risk of a repeat ectopic pregnancy is somewhat increased, but that does not mean it is likely. It mainly means that a new pregnancy should be checked earlier.
Early checks are not panic but prevention. An early ultrasound can quickly provide clarity and is often the most important step to regain reassurance.
Costs and practical planning
Costs and access to care vary greatly by country, insurance system, and care setting. More important than the diagnosis itself is how quickly you can access ultrasound, lab testing, and emergency care.
If you are currently pregnant and have symptoms, the priority is not cost optimization but the fastest safe evaluation. Everything else comes afterward.
Legal and regulatory context
Treatment of ectopic pregnancy is a medical standard worldwide, but specific organization and legal frameworks vary. Differences can include access to emergency care, responsibilities between outpatient clinics and hospitals, documentation requirements, coverage of costs, and in some places rules governing the use of certain medications.
If you are in another country or have cross-border insurance, it is practical to identify the nearest emergency department, which documents you should carry, and who can arrange ultrasound and serial hCG testing on short notice. International rules and responsibilities can differ and may change over time.
Myths and facts about ectopic pregnancy
- Myth: An ectopic pregnancy is caused by improper behavior. Fact: It has medical causes and is not a matter of blame.
- Myth: You always notice an ectopic pregnancy immediately. Fact: Early symptoms can be nonspecific and resemble a normal early pregnancy.
- Myth: Bleeding always means miscarriage. Fact: Early pregnancy bleeding has many causes and must be interpreted in context.
- Myth: If nothing is seen on ultrasound, everything is harmless. Fact: Very early pregnancies are often not yet visible on ultrasound; follow-up and serial testing are important.
- Myth: Surgery is always necessary. Fact: Expectant, medical, or surgical approaches may be appropriate depending on the situation.
- Myth: After an ectopic pregnancy, a normal pregnancy is impossible. Fact: Many people conceive normally afterward, often with earlier monitoring.
- Myth: Pain after treatment is always normal. Fact: Increasing pain, fever, or circulatory problems should be reassessed.
When to seek immediate medical help
Immediate evaluation is necessary for severe lower abdominal pain, shoulder pain, dizziness, fainting, shortness of breath, or heavy bleeding. These may indicate internal bleeding and are a medical emergency.
Conclusion
Ectopic pregnancy is well understood medically but often emotionally distressing. Early assessment, clear diagnosis using serial hCG and ultrasound, and treatment tailored to the individual situation are key. People who take symptoms seriously and seek early evaluation substantially reduce risks.