Artificial Intelligence and Big Data in IVF
Modern embryo scoring programs process time‑lapse videos, lab parameters, and patient data simultaneously. Clinics report that today an embryologist can evaluate three times as many cultures as before – with comparable pregnancy rates.
- Faster Embryo Ranking – optimal blastocyst selection in seconds instead of minutes.
- Personalized Stimulation Protocols – AI takes age, BMI, and hormone profiles into account.
- Continuous Quality Monitoring – algorithms detect incubator anomalies immediately.
Noninvasive Genetic Screening (niPGT-A)
Cell‑free DNA from culture media is increasingly replacing trophectoderm biopsy. The embryo remains intact, and results often arrive in under 24 hours.
- Embryo‑friendly – no additional procedure required.
- Suitable for single‑embryo transfers and preimplantation genetic diagnosis.
- High concordance with traditional PGT‑A while reducing mosaicism rates.
Gene Editing and Gene Therapy Approaches
The FDA approval of the CRISPR therapy Casgevy for sickle cell disease has opened the field. Initial pilot studies are testing whether germline mutations, such as FSH receptor defects, can be repaired before fertilization.
- Germline editing remains strictly regulated, but somatic therapies prior to IVF are under intensive study.
- Mitochondrial replacement (“three‑parent IVF”) is approved in the UK for select couples.
- Ongoing ethical research and independent review boards are now international standards.
Robotics and Laboratory Automation
Pipetting robots, closed incubation systems, and integrated sensor arrays enable nearly autonomous lab operations.
- Consistent conditions for temperature, pH, and oxygen levels.
- Real‑time documentation of all steps – crucial for auditing and traceability.
- Reduced contamination and labor costs.
Microfluidic Sperm Selection
Microchannel chips filter highly motile sperm and minimize DNA fragmentation. Studies show improved blastocyst quality and higher implantation rates.
- Less invasive than gradient or swim‑up methods.
- Particularly useful for couples with a high sperm DNA fragmentation index.
- Compatible with ICSI, IVF, and processed at‑home sperm samples.
Uterus Transplantation as an Option for Uterine Agenesis
Since the first live birth in 2014, more than 70 babies worldwide have been born following a uterus transplant. However, the procedure remains high‑risk and expensive.
- Indications: Mayer‑Rokitansky‑Küster‑Hauser syndrome, hysterectomy due to cancer.
- Risks: preeclampsia, graft rejection, preterm birth.
- Recommended delivery: planned cesarean section from week 37.
3D‑Printed Ovaries and Tissue Engineering
Gel scaffolds made from bio‑ink are already producing functional follicles in mouse models. Clinical trials in humans are still pending, but basic research is advancing rapidly.
- Potential for patients after chemotherapy or radiation therapy.
- Goal: hormonal self‑regulation plus fertility.
- Challenges: vascular integration and long‑term function.
Wearables, Telemedicine, and Fertility Apps
Cycle‑tracking rings, Bluetooth LH tests, and at‑home sperm analyses bring the lab to your smartphone. Fertility clinics now offer complete tele‑IVF packages.
- Real‑time data sharing with treating physicians.
- Lower travel costs and more convenience for couples in rural areas.
- Higher adherence and patient satisfaction.
In Vitro Gametogenesis (IVG) – Artificial Gametes in Focus
Research groups have derived germ cell precursors from human induced pluripotent stem cells. However, many safety assessments are still needed before clinical applications.
- Option for individuals without functional germ cells.
- High ethical and regulatory considerations.
- Unknown long‑term effects on offspring.
Outlook 2030 – Key Trends in the Coming Years
The following developments are likely to shape the fertility treatment market through 2030:
- Polygenic Screening – risk assessment for complex diseases such as diabetes or heart disease before embryo transfer.
- IVF Factories – fully automated production lines with robotic handling and AI quality control.
- Fertility‑on‑a‑Chip – miniaturized labs for sperm analysis and hormone diagnostics for home use.
- Artificial Gametes – IVG could enable genetic parenthood for individuals without their own eggs.
- Digital Ecosystems – integration of cycle trackers, telemedicine, and at‑home insemination kits.
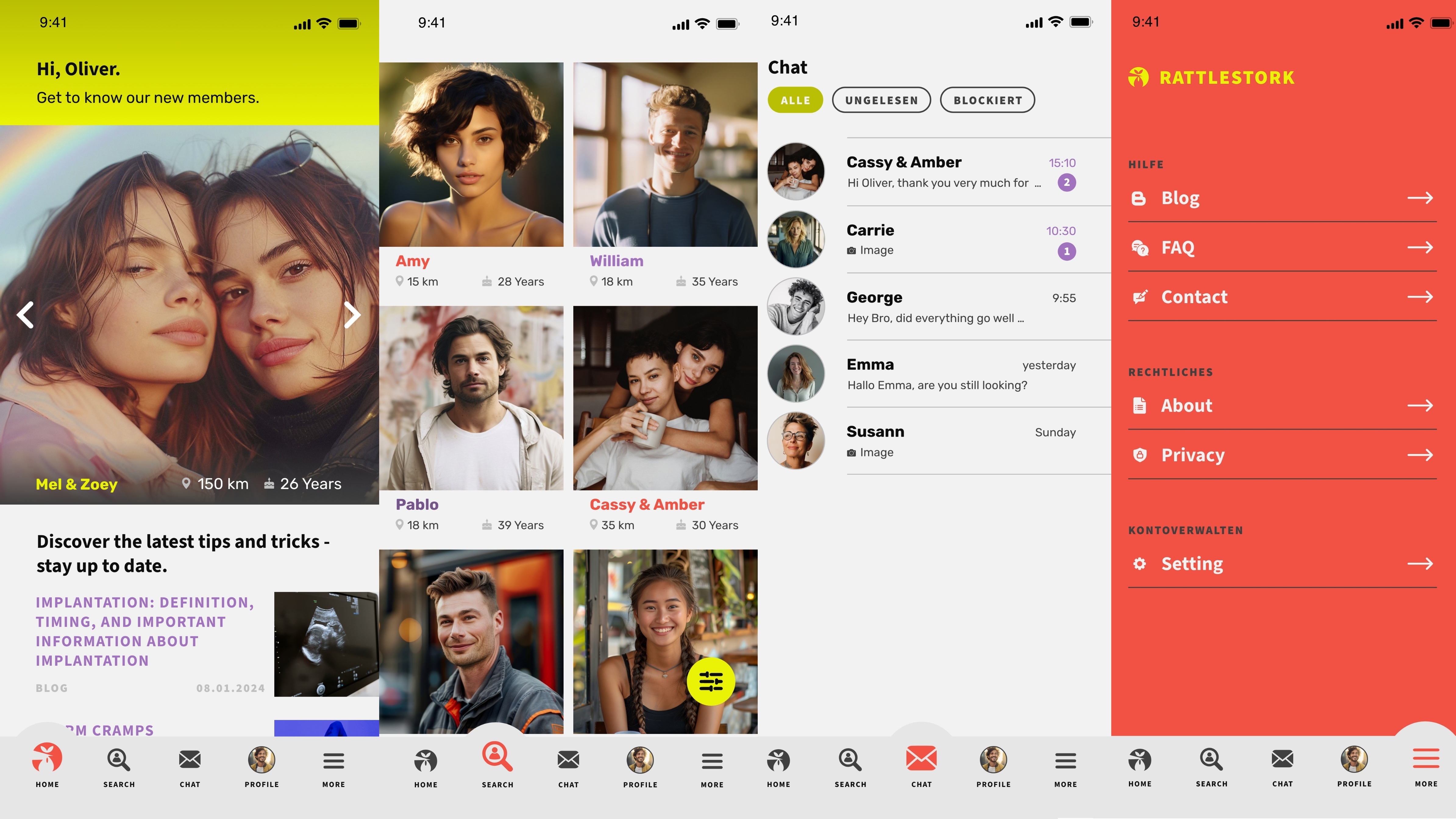
At the same time, according to the WHO Q&A on Human Rights in Reproductive Health, demand is growing for affordable, user‑friendly solutions – a segment already served by app‑based platforms like RattleStork.
Sperm Donation with RattleStork – A Modern Solution without the High‑Tech Price
Not every family needs robots or gene editing. With RattleStork, you can find verified sperm donors and plan a home insemination independently, discreetly, and affordably – all without clinic wait times.
Conclusion
AI embryo scores, robotics labs, and gene therapies represent the cutting edge of reproductive medicine. Simultaneously, low‑barrier options like app‑enabled sperm donation remain essential pillars for making fertility accessible to all. The future lies in an intelligent combination of high‑tech and proven, affordable methods.

