Introduction
Many two-mum couples ask the same question: Which one of us will become pregnant? The answer rarely appears spontaneously. Medical findings, legal requirements, time and budget, day-to-day logistics, and your shared wish all interlock. This guide explains common routes to pregnancy, lays out the key criteria, and links to dependable sources.
Good starting points: NHS: Infertility, NICE guideline CG156, HFEA: Treatment options, ASRM: Preconception counselling, ESHRE: Guidelines.
Paths to parenthood
Depending on country, health, and personal preferences, several routes may fit:
- IUI (intrauterine insemination) in a clinic with prepared donor sperm.
- IVF (in-vitro fertilisation), for example with additional indications or when planning Shared Motherhood.
- Reciprocal IVF / Shared Motherhood: one partner’s eggs, the other carries the pregnancy.
- Home insemination. Medical and legal aspects must be clarified carefully.
- Adoption or co-parenting with a third person or another couple.
Often, a sequence leads to success — e.g., several IUI cycles followed by IVF if needed.
Who carries? Medicine and daily life
Medical work-up for both
Baseline checks include cycle and ultrasound findings, ovarian reserve (AMH/AFC), blood tests, infection screening and, if needed, genetic counselling. In parallel, stabilise sleep, nutrition, activity, and stress management, and start folic acid before conception.
Age and egg quality
Egg age is a strong predictor. It often favours the younger partner providing eggs or carrying the pregnancy. Diagnoses such as endometriosis, fibroids, or thyroid disease can reshape plans and should be assessed clinically.
Health, work, and everyday life
Beyond lab results, practicality matters: chronic conditions, medicines, mental health, working hours, shift work, desire to breastfeed, and your local support network. The guiding question is: Who can realistically handle the physical and time load now — and who wishes to carry to term?
Decision models
- One partner carries the first child; the other carries a second child later.
- Both try to become pregnant around the same time; simultaneous births cannot be guaranteed.
- Reciprocal IVF: partner A’s eggs and partner B carries — or vice versa.
Choosing a donor and the framework
Donor routes include clinic or sperm-bank donation, a known donor in your private circle, or matching platforms. Clinical routes provide lab quality, infection and genetic testing, and clear documentation. With private arrangements, medical tests, written agreements, and the local legal position are critical. Consider expectations about contact, openness, and future information for the child.
Whichever route you choose, a transparent, respectful set-up protects everyone — you, the donor, and the future child.
Reciprocal IVF / Shared Motherhood
The process mirrors standard IVF: stimulation and egg collection for partner A, fertilisation with donor sperm in the lab, and embryo transfer into partner B’s uterus. Success depends mainly on egg age and individual history. Keep a realistic timeline, a clear medicines-and-appointments plan, and awareness of the physical load for both partners.

Advantages: both directly involved; genetic link via the egg-providing partner and the experience of pregnancy for the other. Consider costs, cycle co-ordination, insurance issues, and the legal context. More: HFEA: Reciprocal IVF.
Options at a glance
| Option | In brief | Strengths | Notes |
|---|---|---|---|
| IUI (clinic) | Prepared donor sperm is placed into the uterus. | Strong safety and quality standards; clear documentation. | Plan for multiple cycles; access and costs vary by country. |
| IVF | Fertilisation in the lab; embryo transfer to the uterus. | High control; suitable for more complex findings. | More invasive and costly; requires medical preparation. |
| Reciprocal IVF | Eggs from A; B carries the pregnancy. | Both actively involved; clear roles. | Success closely tied to egg age; check insurance and law. |
| Home insemination | Insemination at home with donor sperm. | Private, flexible, cost-effective. | Without lab screening and documentation, risks rise; clarify legalities carefully. |
More: HFEA clinic finder, NICE CG156.
Safety and tests
Before any route: up-to-date infection screening, vaccination and rubella status, medicines review, start folic acid, and stabilise existing conditions. Clinical pathways also provide sperm preparation, clear lab and documentation chains, and better traceability. NHS, ASRM and ESHRE offer helpful orientation.
Legal basics
Law is country-specific. In many places, the person who gives birth is a legal parent. Whether and how the partner is recognised often depends on status and correctly executed clinic forms. In India, access to assisted reproduction and the assignment of legal parentage are governed by current national laws, rules and clinic practices. As regulations evolve, confirm requirements with your ART clinic and appropriate authorities before you begin.
Starting points: HFEA: Donors and the law, NICE CG156.
Planning: time, money, support
Expect multiple IUI cycles and possible clinic wait times. Check early what your insurance/benefits cover and what you’ll self-fund. Align appointments, working hours, leave and caregiving support across family and friends. Decide who owns which tasks: scheduling, documents, cost tracking, donor or clinic contact.
A simple team checklist: both complete medical work-ups; confirm the legal framework; choose your preferred route; set budget and timeline; prepare contingency and cover plans for daily life.
When to see a doctor
- If pregnancy does not occur after several cycles or cycles are irregular.
- With conditions or medicines that may affect pregnancy.
- Before home insemination to cover screening, safety and legalities.
- Before IVF or Reciprocal IVF to understand success rates, risks and demands.
Myths and facts
- Myth: Home insemination is always the easiest solution. Fact: Without tests and documentation, medical and legal risks increase.
- Myth: Reciprocal IVF guarantees a quick pregnancy. Fact: Chances depend chiefly on egg age and individual findings.
- Myth: The fitter partner should carry. Fact: The decision has many dimensions — medical, legal, time and emotional.
- Myth: Only the birth mother is the “real” mother. Fact: Parenthood can be set out legally and socially; complete the documents and live your model intentionally.
- Myth: Donor sperm means STI tests aren’t needed. Fact: Screening protects you and the child — whichever route you choose.
- Myth: IUI and ICI are equivalent. Fact: Many guidelines prefer IUI over ICI for success rates and process control.
- Myth: Parallel pregnancies can be reliably synchronised. Fact: Biology rules; timing can’t be guaranteed.
- Myth: Reciprocal IVF is always the best emotional choice. Fact: It fits when roles, effort and costs suit you — otherwise there are good alternatives.
- Myth: A known donor makes everything simple. Fact: Clear tests, agreements and legal framing still matter.
- Myth: More stimulation is always better. Fact: Over-stimulation carries risks; dosing follows diagnostics and clinic protocol.
- Myth: After 35 it rarely works. Fact: Chances decline, but individual findings are decisive; good counselling helps interpretation.
- Myth: Law is similar everywhere. Fact: Rules differ widely; always check locally.
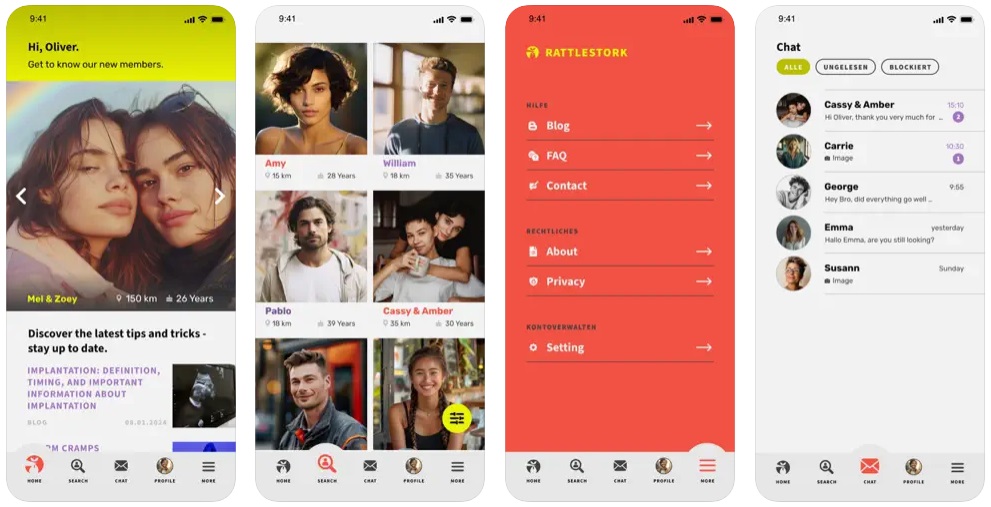
RattleStork – plan transparently
RattleStork supports you with verified profiles, secure messaging, checklists for medical steps and documents, appointment and cycle notes, and an emphasis on open, responsible models. RattleStork does not replace medical advice.
Conclusion
A sound decision sits where medical findings, legal certainty, time and budget meet your shared wish. Gather facts, talk openly, check your local rules and choose the route that fits you.

