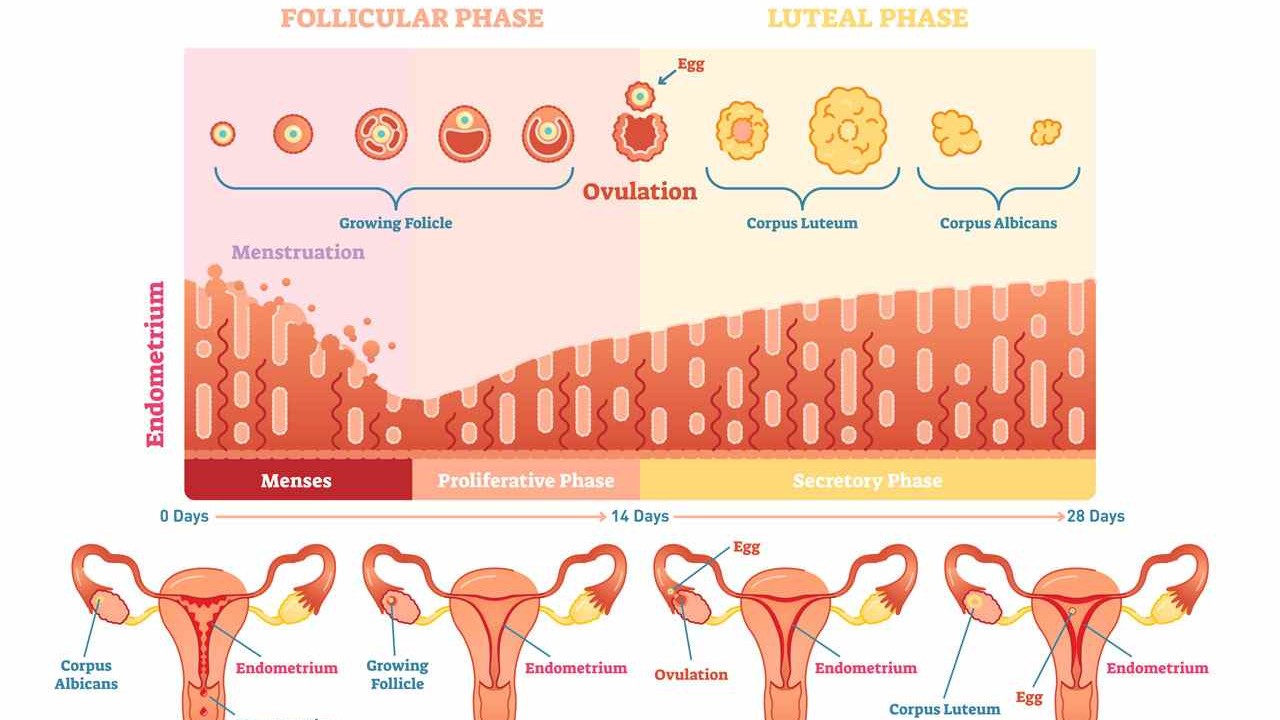
Understanding cycle phases and hormones
- Menstruation (day 1–5): The uterine lining is shed; oestrogen and progesterone are low.
- Follicular phase (day 1 to ovulation): FSH matures a follicle; rising oestrogen rebuilds the lining.
- Ovulation (often day 12–16): The mature egg is released and remains fertilisable for around 12–24 hours.
- Luteal phase (about 14 days): Progesterone from the corpus luteum stabilises the lining. If no pregnancy occurs, levels fall and a new cycle begins.
What is ovulation?
Ovulation is the release of a mature egg from the ovary; fertilisation can then occur in the fallopian tube. On average, ovulation occurs 10–16 days before the next period—so not on the same cycle day for everyone. For reliable patient information, see the NHS overview.
Numbers & evidence
- Egg: fertilisable for roughly 12–24 hours after ovulation (NHS).
- Sperm: can survive up to 5–7 days in the female reproductive tract; the fertile window therefore starts before ovulation (NHS).
- Fertile window: about six days in total, ending on the day of ovulation; highest chances in the two days before and on ovulation day itself (classic data: NEJM Wilcox).
- Everyday recommendation: Intercourse every two to three days reliably covers the window without pinpointing exact dates (NICE CG156).
Calculate fertile days
With regular cycles you can estimate timing: ovulation sits roughly 10–16 days before the next period. Cross-check this estimate with observations or tests—variation is normal.
- Knaus–Ogino rule of thumb: First fertile day = shortest cycle − 18; last fertile day = longest cycle − 11. Orientation only—don’t rely on it alone.
- Reality check: Even with 28-day cycles not everyone ovulates on day 14. Think in windows, not fixed dates (see Wilcox, NEJM).
Methods compared: how to find your window
A lean combo works best: a calendar app for the frame, cervical mucus to predict, basal body temperature to confirm; add an ovulation test if you need precision. That way tracking stays robust and practical.
- Cervical mucus observation: Clear, stretchy mucus indicates high fertility. Low cost, needs a little practice (NICE guidance).
- Basal body temperature (BBT): Measure on waking. The rise confirms ovulation retrospectively—good for confirmation, less for advance planning (NICE).
- Ovulation predictor kits (OPKs): Detect the surge that precedes ovulation; provide a 12–36 hour action window.
- Calendars/apps: Useful for patterns and reminders, but only estimates if cycles fluctuate.
Ovulation tests: quick & correct use
- Start four to five days before your earliest likely ovulation date.
- Use the second morning urine (concentrated, but not collected overnight).
- Test at the same time daily and follow the manufacturer’s instructions exactly.
- If positive: plan intercourse the same day and the day after.
If tests are repeatedly unclear, a progesterone blood test can confirm ovulation (NICE CG156).
Typical symptoms
- Glassy, stretchy cervical mucus
- Mild one-sided lower-abdominal pain (mittelschmerz; not present for everyone)
- Subtle temperature rise the following day (BBT)
Many feel no clear signs. Rely on the combination of observations and testing rather than “gut feel”.
Practical tips
- Low-pressure timing: intercourse every two to three days reliably covers the window (NICE CG156).
- Routine: assess mucus at the same time each day; measure BBT immediately after waking.
- Lifestyle: don’t smoke, avoid alcohol, sleep sufficiently, eat a balanced diet—solid, guideline-backed basics (NICE).
Comparison table: which method for what?
| Method | Use | Strength | Limitation |
|---|---|---|---|
| Cervical mucus | Predicting the fertile phase | Free, immediate | Interpretation needs practice |
| Basal body temperature | Confirmation after ovulation | Low cost, objective | Not predictive; daily measuring needed |
| OPK (ovulation test) | Short-term planning (12–36 h) | Concrete action window | Cost; correct testing window is crucial |
| Calendar/app | Framework & trend | Good overview | Only an estimate if cycles vary |
Myths & facts about ovulation
- “Ovulation is always on day 14.” Ovulation day varies widely, even in 28-day cycles. Think in windows (NEJM Wilcox).
- “No mittelschmerz means no ovulation.” Many feel nothing and still ovulate normally (NHS information).
- “BBT predicts ovulation.” It confirms it afterwards; for planning, mucus observation and OPKs are more suitable (NICE guidance).
- “Daily sex boosts chances dramatically.” Every two to three days is sufficient and less stressful (NICE).
- “Apps pinpoint ovulation exactly.” They estimate. Individual variance remains; combining with body signs/OPKs is more reliable.
- “No positive test means no ovulation.” You may have missed the testing window; a progesterone blood test can confirm it (NICE).
- “I’m only fertile on ovulation day.” Sperm can survive up to seven days; the fertile phase starts before ovulation (NHS).
- “Irregular cycles equal infertility.” Fluctuations are common. What matters is whether ovulations occur; see a clinician if unsure.
Irregular cycles: when to see a clinician
If your cycles vary greatly, periods stop, or ovulation remains unclear despite tracking, seek assessment. Common causes include thyroid disorders, PCOS, extreme weight or marked stress. Clinicians can confirm ovulation with a progesterone blood test; see NICE CG156 for guidance. For background on infertility, the WHO fact sheet is helpful.
Conclusion
The egg is fertilisable for only 12–24 hours; sperm can survive up to 5–7 days. What matters most is the window before ovulation and the day itself. A calm combination of a cycle app, cervical-mucus observation, BBT for confirmation and—if needed—an OPK reliably gets you there. If conception doesn’t happen or cycles are irregular, early guideline-based assessment helps.

