Why a multi-stage screening is essential
Many pathogens have a window period: shortly after infection an antibody test may still be negative while PCR/NAT can already detect the agent. That is why reputable programmes combine medical history, serological tests, PCR/NAT and a delayed release after repeat testing (commonly 90–180 days). This approach significantly reduces the residual risk. The logic follows framework recommendations from ESHRE and public health authorities such as MoHFW/ICMR.
Viruses that can be detectable in ejaculate
- HIV – antigen/antibody combination test plus PCR/NAT; release only after a second blood sample.
- Hepatitis B and C – HBsAg, anti-HBc, anti-HCV and HCV-NAT; chronic infections must be reliably excluded.
- CMV – IgG/IgM and PCR if indicated; relevant in pregnancy.
- HTLV I/II – rare, screened in many programmes.
- HSV-1/2 – clinical history, PCR if suspected.
- HPV – PCR for high-risk types; positive samples are discarded.
- Zika, Dengue, West Nile – travel history, where appropriate RT-PCR and deferral after stays in endemic areas.
- SARS-CoV-2 – now mainly history and symptom checks; programme requirements vary.
Bacteria and parasites in the context of sperm donation
- Chlamydia trachomatis – often asymptomatic; NAAT from urine or swab.
- Neisseria gonorrhoeae – NAAT or culture with resistance testing.
- Treponema pallidum (syphilis) – TPPA/TPHA and activity markers (e.g., VDRL/RPR).
- Trichomonas vaginalis – NAAT; can impair sperm function.
- Ureaplasma/Mycoplasma – treat specifically if detected.
- Uropathogenic bacteria (e.g., E. coli, enterococci) – culture if suspected; problematic strains are excluded.
Genetic risks: what is standard today
- Cystic fibrosis (CFTR)
- Spinal muscular atrophy (SMN1)
- Haemoglobinopathies (sickle cell, thalassaemias)
- Fragile X (FMR1) depending on history
- Y-chromosome microdeletions in severe oligo/azoospermia
- Population-specific panels (e.g., Gaucher, Tay–Sachs)
Expanded testing is guided by family history and ancestry. ESHRE recommends transparent definition of indication areas.
Risk matrix: pathogen, test, window period, release
| Pathogen | Primary test | Window period | Typical release | Note |
|---|---|---|---|---|
| HIV | Ag/Ab combo + PCR/NAT | Days to a few weeks | After retest (90–180 days) | NAT reduces uncertainty |
| HBV/HCV | HBsAg, anti-HBc, anti-HCV, HCV-NAT | Weeks | After retest | Check HBV vaccination status |
| Syphilis | TPPA/TPHA + activity markers | 2–6 weeks | Only if full serology negative | Treatment → deferral until resolved |
| Chlamydia/Gonorrhoea | NAAT (urine/swab) | Days | If negative | Positive → treatment, test of cure |
| CMV | IgG/IgM ± PCR | Weeks | Bank-dependent | Relevance in pregnancy |
| Zika/West Nile | RT-PCR + travel history | Weeks | Deferral after travel/infection | Consider endemic areas |
Specific timeframes vary by laboratory and national regulations. Guidance is provided by ESHRE, national public health authorities (e.g., MoHFW/ICMR) and applicable tissue/cell regulations.
How the screening process works
- Medical history and risk assessment – questionnaire, travel and sexual history.
- Laboratory tests – combination of antibody/antigen and PCR/NAT.
- Genetic panel – according to guidelines and history.
- Quarantine – freezing and delayed release after retesting.
- Final release – only with completely normal results.
Private sperm donation: how to stay safe
- Current written test results from both parties (HIV, HBV/HCV, syphilis, chlamydia/gonorrhoea; depending on circumstances CMV, trichomonas).
- No unprotected sex with third parties during the window period after tests.
- Use sterile disposable containers only, clean surface, wash hands; do not mix samples.
- Document date, time and test results; record agreements in writing.
- If symptoms such as fever, rash or discharge occur, postpone donation and seek medical review.
Medical background on STI prevention: CDC and national public health authorities provide layperson-friendly overviews.
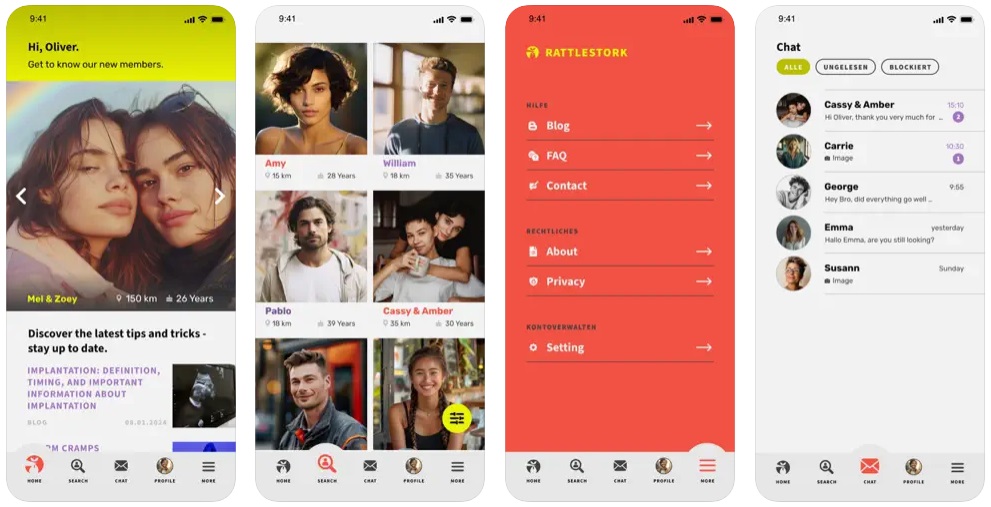
Sperm donation with RattleStork: organised, documented, safety-minded
RattleStork helps you plan a private sperm donation responsibly. You can exchange test results securely, set reminders for retests, use checklists for disposable materials and document individual consents. Our practical checklist guides preparation, clean collection and handover. This keeps the donation planned and transparent while maintaining safety standards.
Law and standards (India / international)
In India, collection, testing and release of donor gametes follow national regulations and guidance from bodies such as the Ministry of Health and Family Welfare (MoHFW) and the Indian Council of Medical Research (ICMR). Facilities may also refer to international standards like ESHRE and relevant tissue/cell directives. Many banks additionally limit the number of children per donor and maintain registries.
Conclusion
Reputable sperm banks combine medical history, serological tests, PCR/NAT, quarantine and retesting. This makes infections and genetic risks very rare. The same principles are essential for private donations: up-to-date tests, observing window periods, hygiene, documentation and clear agreements. RattleStork provides structured support for a safe, responsible sperm donation.

