Ovarian reserve (AMH & AFC) – your biological "savings account"
The number of follicles is set at birth and declines over life. Two measures give a useful overview of the remaining reserve today:
- AMH (anti-Müllerian hormone): a blood value that reflects the size of the active follicle pool. Low AMH suggests a smaller reserve, high AMH a larger one.
- AFC (antral follicle count): ultrasound counting of small follicles at the start of the cycle; together with AMH it is informative for planning.
| Measure | What it shows | Typical use |
|---|---|---|
| AMH | Size of the follicle pool | Screening, monitoring over time, stimulation planning |
| AFC | Number of visible antral follicles | Cycle-start ultrasound, reserve estimation |
| FSH (day 2–5) | Pituitary regulation | Elevated = sign of reduced reserve |
Interpretation should be done by experienced clinicians. Guidelines recommend structured assessments before treatment decisions.
Age & egg quality: what happens in the ovary
- Chromosome distribution: with increasing age aneuploidies rise, which increases miscarriage risk and can make implantation harder.
- Mitochondria & energy: eggs of older women often have fewer "energy reserves", which can affect early embryo stages.
- Hormonal dynamics: cycle phases may shorten; the "window" for implantation can become smaller.
- Overall effect: reduced reserve and reduced egg quality explain why additional support is often helpful from the mid to late 30s.
Numbers & success rates – realistic expectations
Natural chance per cycle: roughly 25–30% under 30, 10–15% at 35 and frequently < 5% from 40. These ranges vary with cycle regularity, partner sperm and pre-existing conditions.
Miscarriage risk: increases with age (aneuploidies). Individual counselling is advisable, especially after repeated miscarriages.
IVF/ICSI: age-dependent success rates are reported in national registries; good overview data is available from the CDC ART National Summary and other registries.
Strengthening egg quality – effective levers
- Quit smoking: tobacco accelerates ovarian ageing; stopping smoking pays off immediately.
- Weight & metabolism: aim for a stable BMI in the normal range and good insulin sensitivity.
- Alcohol & environment: avoid heavy consumption; reduce exposure to endocrine disruptors (BPA/plasticisers).
- Sleep & shift work: regular sleep times improve hormonal balance.
- Exercise & stress management: moderate exercise, breathing and relaxation techniques.
- Partner check: a semen analysis clarifies whether male factors contribute.
Guidelines emphasise lifestyle interventions as the foundation — treatment options build on these (see NICE, NHS).
Testing fertility – AMH, AFC & cycle tracking
- AMH blood test: reserve marker; sensible as a baseline from the early 30s and then repeated periodically.
- AFC ultrasound: counting antral follicles at cycle start; very useful together with AMH.
- Cycle tracking: urine LH tests, basal temperature, cervical mucus or wearables to hit the fertile window.
- Additional diagnostics depending on findings: thyroid, prolactin, insulin resistance, vitamin D, coagulation; investigate for endometriosis if suspected.
Guidance: under 35 seek medical advice after 12 months without pregnancy, from 35 after 6 months (recommendations e.g. NHS).
Social freezing – process, chances & costs
Process
- 10–12 days of stimulation with daily injections
- Monitoring with ultrasound and hormone values
- Follicle retrieval under short anaesthesia (≈ 15 minutes)
- Vitrification at −196 °C
Success chances
The younger the eggs at freezing, the higher the later chance per egg. Under 35, target ranges of about 12–20 eggs are often discussed; with increasing age the success probability per egg decreases. Ethical and medical aspects: ESHRE guidance.
Costs
- Stimulation cycle: approx. €3,000–4,500
- Storage per year: approx. €200–300
- Reimbursement usually only for medical indications
To put success rates in context, consult national registries and international data such as the CDC data.
Pre-existing conditions & risks – when to look more closely
Factors that can play a role include endometriosis (adhesions, pain), PCOS (ovulatory disorders, insulin resistance), thyroid dysfunction, hyperprolactinaemia, coagulation disorders (e.g. Factor V Leiden). If you have irregular cycles, severe pain, repeated miscarriages or more than 6–12 months of unsuccessful attempts, consider referral to a fertility clinic.
Your plan from today
- Baseline check: have AMH & AFC measured in the coming weeks.
- Sharpen timing: track 2–3 cycles with LH tests + basal temperature.
- Leverage lifestyle: stop smoking, regular sleep, exercise, nutrition, reduce alcohol.
- Clarify options: spontaneous attempts vs. IUI/IVF, possibly social freezing; arrange personalised counselling.
- Check partner factor: plan a semen analysis if appropriate.
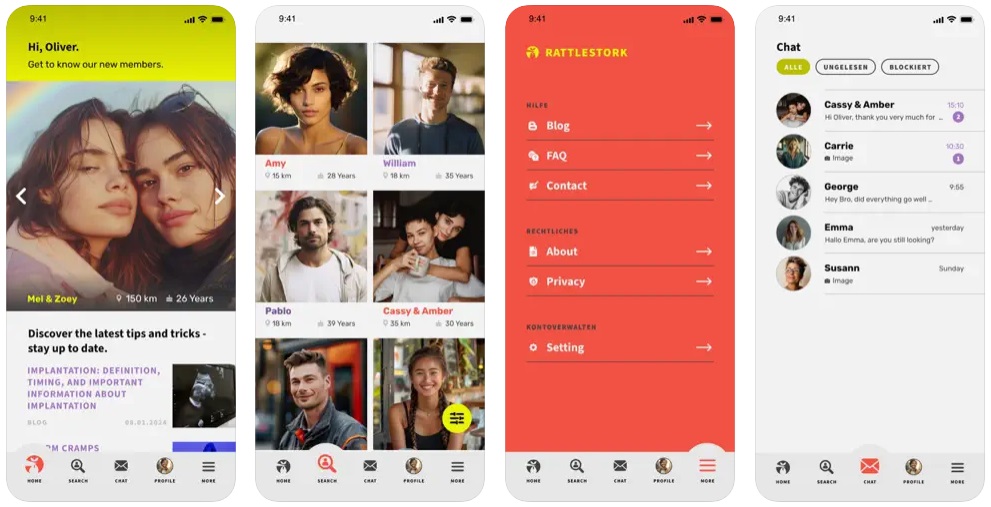
Sperm donation with RattleStork – an option without a partner
If a partner is absent or male factors are limiting, you can discover verified donor profiles via the RattleStork app, make contact and plan procedures — from anonymous donation to co-parenting or home insemination. This helps you make informed decisions suited to your situation.
Conclusion
You cannot stop time — but you can use it. Knowing your reserve and risks, optimising timing and soberly evaluating options like social freezing or assisted reproduction measurably improves the chances. For orientation and planning consult national guidance (MoHFW/ICMR) and international sources such as WHO, NICE, NHS, CDC ART and ESHRE.