At a glance
During the pandemic, bold claims about “unvaccinated vs vaccinated sperm” circulated widely. The research consensus is clear: COVID‑19 vaccines do not cause lasting changes in semen quality. Studies find no clinically relevant differences in concentration, motility, morphology, or DNA integrity. A COVID‑19 illness can temporarily lower values—typically recovering within weeks to a few months. For reliable guidance, see the CDC, RKI, WHO and Swissmedic.
Semen quality – basics
Four key metrics guide the assessment of male fertility:
- Concentration – sperm per millilitre of ejaculate
- Motility – movement and forward progression
- Morphology – proportion of normally‑shaped sperm
- DNA integrity – intactness of genetic material
These metrics are sensitive to fever, acute illness, scrotal heat, tobacco and alcohol, excess weight, stress, and certain environmental exposures.
Evidence on vaccination
Prospective studies and longitudinal observations show no deterioration of semen parameters after mRNA vaccination. A JAMA analysis with measurements before and after two doses found stable values for volume, concentration, motility and morphology (Gonzalez et al., 2021). Systematic reviews and meta‑analyses confirm this across platforms (Ma et al., 2023; Li et al., 2023).
Regulatory conclusion: there is no signal of a fertility risk for men from COVID‑19 vaccines (see the CDC, WHO, Swissmedic).
Infection vs vaccination
Infection: After COVID‑19 illness, temporary decreases have been reported—lower concentration and motility, sometimes higher DNA fragmentation. Values usually recover within weeks to a few months.
Vaccination: For mRNA, vector and inactivated vaccines, studies show no clinically relevant negative effects on semen parameters. Short‑term fluctuations with fever are possible and resolve.
Myths and fact‑check
- “Vaccines cause infertility.” False. Authorities including CDC, WHO, RKI and Swissmedic find no evidence of fertility harm. Infection is the bigger risk.
- “mRNA changes DNA or germ cells.” False. mRNA remains in the cytoplasm and is degraded quickly; genomic integration is not biologically plausible.
- “Antibodies attack the placenta/syncytin‑1.” False. There is no robust evidence of clinically relevant cross‑reactivity.
- “Unvaccinated sperm is more valuable.” False. What matters is quality (concentration, motility, morphology) and medical screening—not vaccination status.
- “Boosters worsen semen quality.” False. Follow‑up data show no additional negative effects; short‑term fever‑related changes normalise.
- “Testosterone drops after vaccination.” False. Studies do not show sustained, clinically relevant hormonal changes.
- “Antibodies in semen are harmful.” False. Transient antibodies can be measurable but do not imply functional loss.
- “Some manufacturers are worse for fertility.” False. Comparisons show no relevant differences among authorised vaccines.
- “You should bank sperm before vaccination.” False. Not generally recommended for healthy men; exceptions apply in other risk contexts (e.g., oncology).
Zeitgeist & protest culture
The “unvaccinated vs vaccinated sperm” debate became a meme and political slogan. At protests the line “Unvaxxed sperm is the next Bitcoin” appeared—provocative, catchy, and built to go viral. It shows how quickly punchlines can crowd out facts.

Source & licence: Flickr photo page • Creative Commons BY 2.0
Context helps: viral slogans are not evidence. The data show no lasting disadvantages of vaccination for semen parameters. The supposed “market value” of unvaccinated sperm is unfounded—quality and medical screening are what matter.
Long‑term & platforms
Longer follow‑ups and overviews show no clinically relevant effects on semen parameters. Mechanistically, vaccines do not enter germ cells; there is no plausible pathway for lasting damage. National assessments report no fertility safety signal.
Lifestyle & environment
- Reduce heat: avoid tight trousers, very hot baths, frequent sauna, and laptops on the lap
- Limit tobacco and alcohol: lower oxidative stress and DNA damage
- Diet and exercise: vegetables, fruit, omega‑3 sources, regular activity; manage excess weight
- Stress and sleep: reduce chronic stress, stabilise sleep quality
- Minimise exposures: pesticides, solvents, heavy metals—observe workplace safety
Practice: semen analysis & check‑ups
A WHO‑standard semen analysis remains the basic diagnostic. After acute illness or fever, wait one full maturation cycle (about 72–90 days) before re‑testing. For family planning, the CDC offers concise, accessible guidance on vaccination and fertility.
- Preparation: two to seven days of sexual abstinence
- Laboratory: accredited andrology or urology service
- Follow‑up: in case of infertility, repeat tests every three to six months
- Counselling: urology or andrology for result interpretation, lifestyle coaching and therapy if needed
Comparison table
| Aspect | Vaccination | COVID‑19 illness |
|---|---|---|
| Sperm concentration | No clinically relevant changes (studies/reviews) | May be temporarily reduced; recovery in weeks to months |
| Motility & morphology | No clinically relevant effects | Temporary decreases, recovery over time |
| DNA integrity | No evidence of damage | Some reports of higher fragmentation after acute illness |
| Regulatory view | No fertility signal (CDC, WHO, Swissmedic) | Illness as a short‑term stressor on spermatogenesis |
Official positions
Public authorities reach the same conclusion: there is no indication of vaccine‑related impairment of male fertility. Useful summaries: CDC, RKI, WHO and Swissmedic.
When to see a doctor
Medical evaluation is advisable if any of the following apply:
- Infertility after 12 months (after six months from age 35)
- Abnormal semen analysis or symptoms such as pain, swelling, or signs of infection
- Persistent fever, testicular injury, or known testicular/vasal disease
- Planned chemo‑ or radiotherapy—discuss fertility preservation early
RattleStork – Planning and community around sperm donation
RattleStork helps people plan family‑building responsibly. The platform offers verified profiles, protected conversations, and practical tools for organisation—appointment notes, cycle and timing entries, plus private checklists. RattleStork does not replace medical or legal advice, but bundles information and makes it easier to find suitable contacts.
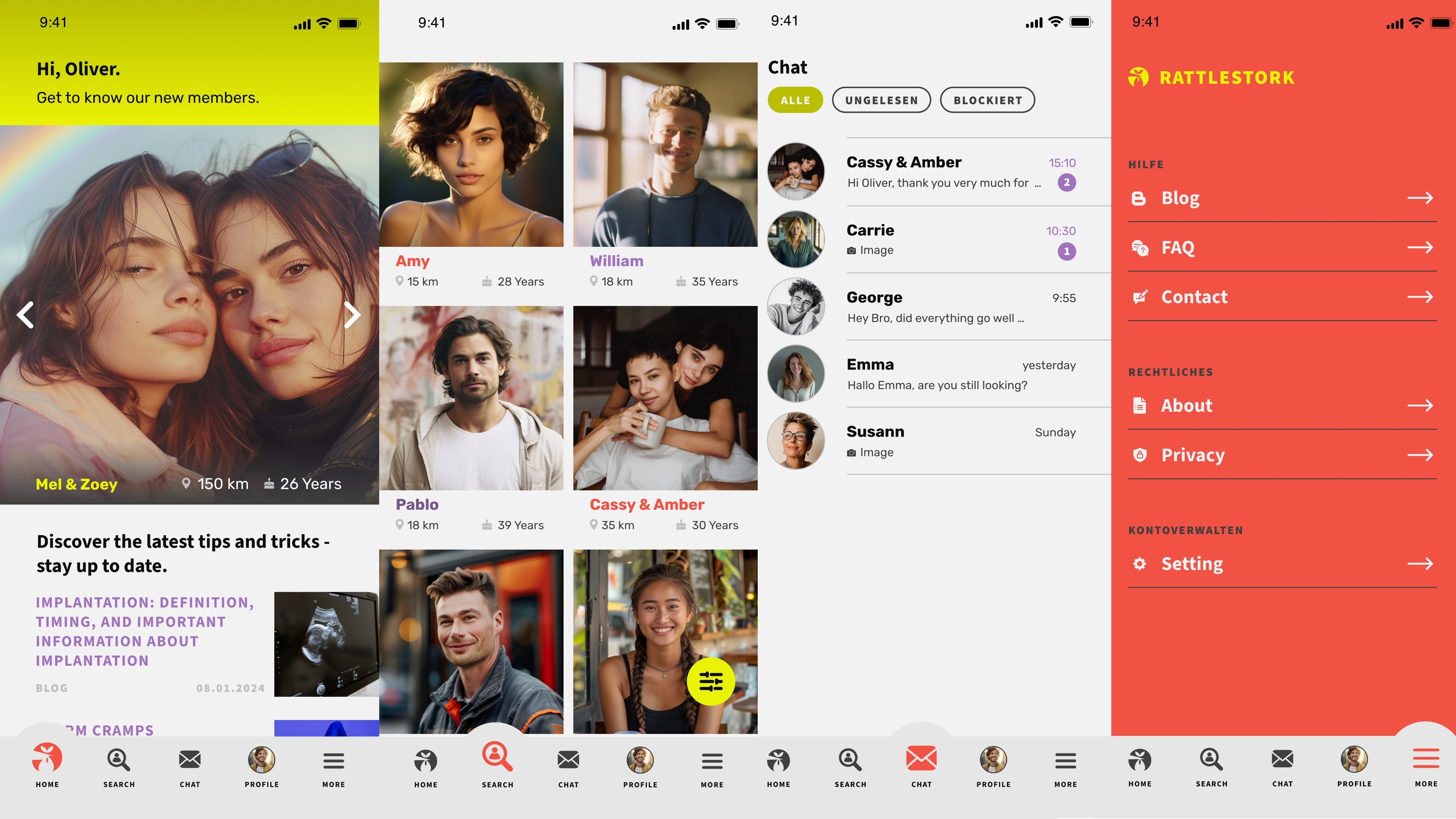
[Fun] If you are determined to look for “unvaccinated sperm”, you can compare profiles with health information on RattleStork—of course without any guarantee and only within medical, data‑protection and personality‑rights boundaries. We do not vouch for user statements; medical tests and the consent of all parties are always required.
Conclusion
The evidence is consistent: COVID‑19 vaccination does not harm semen quality. For male fertility, the drivers are infections (including fever), heat, lifestyle and environmental factors. If you are actively planning, focus on prevention, healthy routines and standard diagnostics—not the vaccination status of semen.

