What the phrase really means
It does not involve a kitchen baster. In practice, it means collecting fresh semen in a sterile, wide-mouth cup and placing it close to the cervix with a small, needle-free syringe. In clinical language this is closest to intracervical insemination (ICI) done at home. A kitchen baster is oversized, not sterile, and unsafe for bodies.
Key facts that matter
- The fertile window spans the days before ovulation; ovulation typically occurs about 10–16 days before the next period. See preconception basics via PregnancyInfo.ca (SOGC).
- Many conceive within a year with well-timed attempts; age and health conditions change the timeline. Canadian guidance emphasises healthy habits and folic acid.
- Helpful habits: time by LH surge, avoid smoking, keep a healthy weight, and start a prenatal with folic acid (commonly 400 µg/day unless advised otherwise).
Safety and hygiene
- Use new, single-use syringes and a sterile collection cup. Avoid saliva and non–sperm-safe lubricants; some products reduce motility.
- Use the sample within about an hour at room temperature (roughly 20–25 °C). Keep surfaces clean and wash hands.
- If using banked donor sperm shipped for home ICI, Canadian establishments operate under the Safety of Sperm and Ova Regulations (SOR/2019-192) for screening, testing and traceability (see Justice Laws).
Supplies checklist
- Sterile, wide-mouth collection cup
- Small needle-free medical syringe (5–10 mL; catheter-tip or slip-tip)
- Ovulation predictor tests (LH strips or digital)
Optional: disposable gloves and a lubricant labelled fertility-friendly.
At-home steps most people follow
- Collect semen in the sterile cup (no condoms or saliva).
- Let it stand at room temperature for 10–15 minutes to liquefy.
- Draw it up slowly and tap out air bubbles.
- Lie comfortably with hips slightly elevated. Place the syringe tip just inside the vagina and angle toward the cervix about 2.5–5 cm (1–2 inches).
- Press the plunger gently and rest for 15–20 minutes.
Stop if anything feels painful or uncertain and contact a clinician.
Timing that helps
- Use LH tests as you approach mid-cycle. Many aim for the evening of the first positive result and, if desired, repeat once 12–24 hours later.
- The fertile window is roughly the five days before ovulation and the day of ovulation; preconception care in Canada emphasises steady habits and folic acid.
Alternatives and how they differ
- Clinic IUI with donor sperm: adds screening, consent and medical oversight; Canadian donor establishments follow federal safety/traceability rules (SOR/2019-192).
- Timed intercourse with a partner: uses the same fertile-window logic and is often a first step before investigations guided by your clinician.
Canadian legal basics you should know
The federal framework comprises the Assisted Human Reproduction Act (AHRA) and the Safety of Sperm and Ova Regulations. The AHRA prohibits paying for donor sperm/ova and regulates related activities (overview at Health Canada). The Safety Regulations set out donor screening, testing, records and error/accident reporting for establishments that process and distribute donor sperm/ova (Justice Laws). Parentage is provincial/territorial and can differ, especially with known donors; review your province’s rules and consider local legal advice before proceeding.
When to see a clinician
- Under 35 and not pregnant after 12 well-timed cycles
- Aged 35+ and not pregnant after 6 cycles
- Right away for very irregular cycles, suspected anovulation, endometriosis, PCOS, thyroid disease, recurrent pregnancy loss, or any safety concerns
Preconception care in Canada also emphasises folic acid and routine health checks before trying to conceive (see PregnancyInfo.ca).
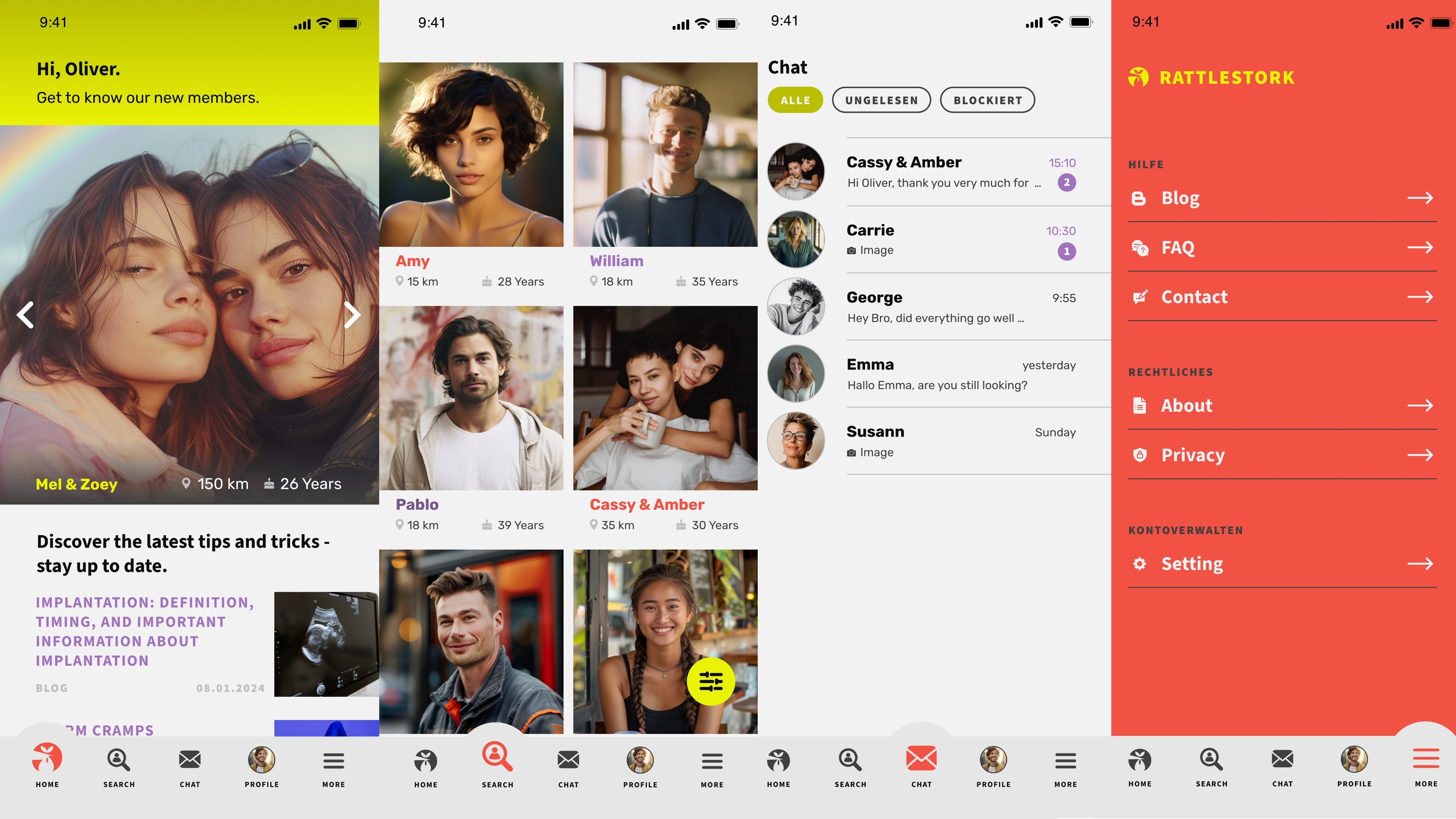
Find verified donors with RattleStork
RattleStork helps intended parents in Canada connect with verified donors, agree clear boundaries, and plan syringe-based attempts with simple checklists and transparent expectations. Start a conversation, review safety tips, and move at your own pace.
Myths and facts
- Myth: A kitchen turkey baster works. Fact: it is unsafe and unsuitable; use a small medical syringe.
- Myth: Any lube is fine. Fact: many lubricants reduce sperm motility; choose fertility-friendly products.
- Myth: Legs-up guarantees success. Fact: timing around ovulation is what matters.
- Myth: Home attempts remove legal risk. Fact: parentage rules are provincial/territorial; know them before you proceed (federal backdrop: AHRA and Safety Regulations).
Conclusion
In Canada, “turkey baster pregnancy” is slang for syringe-based at-home attempts. If you explore this path, keep it clean and simple, time around ovulation, and understand both federal rules (AHRA/Safety Regs) and your province’s parentage law. If progress stalls or you prefer medical oversight, speak with a clinician about testing, clinic IUI or other next steps.

