Why Transparency Strengthens Your Family
Long-term studies show that children who learn about their conception via sperm donation before age seven report stronger trust in their parents and fewer identity conflicts as young adults. The WHO’s Nurturing Care Framework emphasizes that a secure early bond is the foundation for lifelong resilience.
The Right Time: Start Early & Build Gradually
Begin in the preschool years with simple phrases like, “A kind person helped us with special cells.” By elementary school, your child should understand that a sperm donor was involved. The WHO fact sheet on Adolescent Mental Health recommends open communication to prevent later identity crises.
Parental Mindset: Three Steps to Prepare
- Reflect on your own feelings: Write down doubts, fears, and hopes, and discuss them with your partner or a counselor.
- Draft your story: “We wished for a child → sought medical help → a generous donor made it possible.”
- Gather keepsakes: Ultrasound photos, clinic snapshots, or neutral diagrams to make the conversation tangible.
Age-Appropriate Examples for Five Stages
- 0–3 years: “You were our special wish come true.”
- 4–6 years: “A kind person gave us special cells.”
- 7–10 years: Basic facts about egg and sperm cells, and the child’s right to know their origins.
- 11–14 years: Allow questions about feelings, discuss identity and privacy.
- 15+ years: Emphasize self-determination, explain options for donor contact.
Psychological Support—When to Seek Professional Help
Most children adjust well, but reach out if you notice:
- Withdrawal from friends or family
- Persistent guilt or shame
- Depression, eating issues, or school problems
Free support is available through the national Donor Conception Coordination Center (BKiD), the Donor‐Conceived Network, or local family and couples counseling services.
Genetic Health & Donor Records
Later on, your child may need access to key medical details about the donor:
- Negative tests for HIV, hepatitis B/C, syphilis, chlamydia
- Blood type and Rh factor
- Family history of inherited conditions (e.g., cystic fibrosis)
- Basic physical traits (height, hair color, eye color)
Store scans of these records in a secure, password-protected cloud folder and note the donor code. At the legally specified age, your child can request further information directly.
Half-Sibling Networks & Making Contact
Platforms like the Donor Sibling Registry (DSR) let families connect with genetic half-siblings—or choose to stay anonymous:
- Create an account: Register using the donor code.
- Choose your privacy level: Receive only match alerts or open direct communication.
- Shape the contact: Start with email, then video, and meet in person only with mutual agreement.
Answering Tough Questions with Confidence
- “Do I have two dads?”
Explain the difference between social parenting and biological contribution. - “Can I meet the donor?”
Clarify age limits and registration procedures. - “Will I look like them?”
Genetics may influence appearance, but identity is much more.
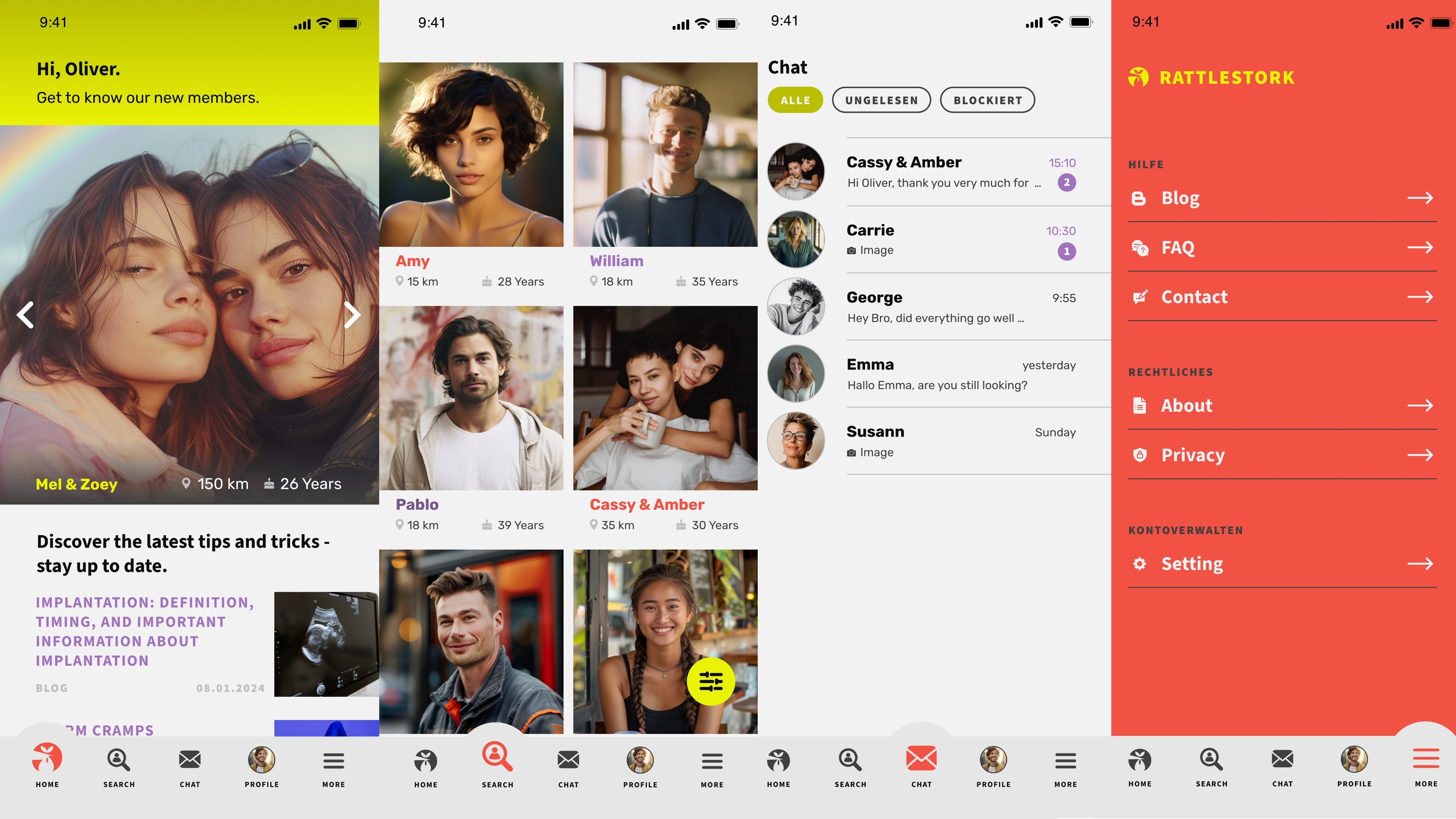
RattleStork—Find Verified Donors & Supportive Community
RattleStork safely connects intended parents with vetted donors and offers an active community where families share their experiences.
Conclusion
Open, age-appropriate conversations about sperm donation build trust and self-esteem. By using the right resources, seeking help when needed, and taking it step by step, you’ll guide your child toward a strong, positive sense of identity.

